Key facts
Why is it important?
Aboriginal and Torres Strait Islander people currently experience higher levels of morbidity and mortality from potentially avoidable conditions than other Australians (see measure 1.24 Avoidable and preventable deaths). Exposures to risk through behaviours such as smoking were also higher (see Health Behaviours measures).
Health promotion is the process of enabling people to increase control over their health and its determinants, and thereby improve their health (WHO 2008). Health promotion activities are designed to improve or protect health within social, physical, economic and political contexts. Health promotion includes public policy interventions (e.g., packaging of tobacco products and seat belt laws), information to support healthy lifestyles (e.g., smoking, alcohol and drug use, physical activity and diet), social marketing (e.g., sunscreen and safe sex) and mass media campaigns (e.g., drink-driving and road safety). Health promotion also includes empowering individuals, strengthening community capacity and addressing determinants of health. It embraces not only actions directed at strengthening the skills and capabilities of individuals but also actions directed towards changing social, environmental and economic conditions to alleviate their impact on public and individual health (WHO 2008).
Currently there are limited methods for measuring the nature, level, and reach of health promotion programs and activities.
Data findings
Health promotion funding
Estimating expenditure on health promotion for Indigenous Australians is difficult since it is often embedded within other funding sources and programs (e.g., funding for general practitioners—GPs, primary health care and mainstream health promotion activities). In 2015–16 it was estimated that state and territory government public health expenditure for selected health promotion services was almost twice as high for Indigenous Australians compared with non-Indigenous Australians ($41 per Indigenous Australian and $21 per non‑Indigenous Australian). In addition, expenditure for the prevention of hazardous and harmful drug use was estimated to be $26 per Indigenous Australian compared with $4 per non-Indigenous Australian (Table D3.03.1, Figure 3.03.1).
Figure 3.03.1: State and territory government health expenditure for Indigenous and non-Indigenous Australians on core public health services, 2015–16
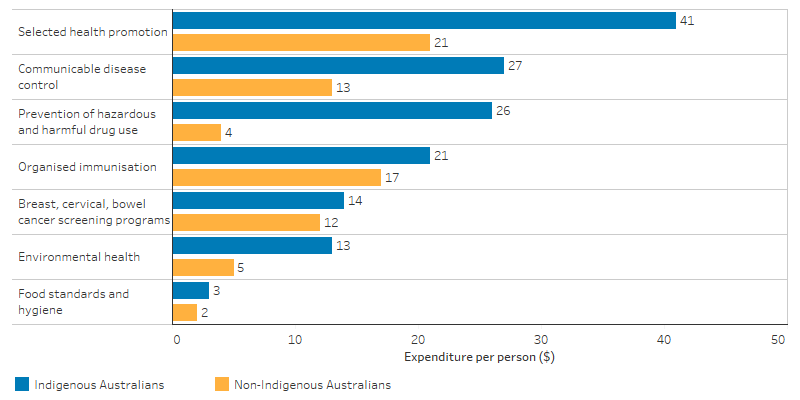
Source: Table D3.03.1. AIHW health expenditure database.
Australian Government funding for core public health services was $180 per Indigenous Australian, this was 2.3 times the amount of funding for non-Indigenous Australians ($77 per person) (Table D3.03.1). This includes a broad set of activities from which health promotion could not be separated.
Lifestyle issues discussed with a doctor
The 2018–19 National Aboriginal and Torres Strait Islander Health Survey showed that 47% of Indigenous Australians aged 15 and over who had consulted a doctor in the last 12 months reported discussing lifestyle issues. These included reaching a healthy weight (48%), eating healthy food or improving their diet (42%), reducing or quitting smoking (37%), increasing physical activity (32%), drinking alcohol in moderation (16%), safe sexual practices (10%) and family planning (8%) and drug use (4%) (Table D3.03.3).
Indigenous females (49%) were more likely to have discussed lifestyle issues with a general practitioner (GP) than Indigenous males (44%). Discussions on drinking alcohol in moderation were more common for Indigenous males (24%) compared with Indigenous females (10%) (Table D3.03.3, Figure 3.03.2).
Figure 3.03.2: Whether discussed health lifestyle issues with doctor or health professional, Indigenous Australians aged 15 years and over, by sex, 2018–19
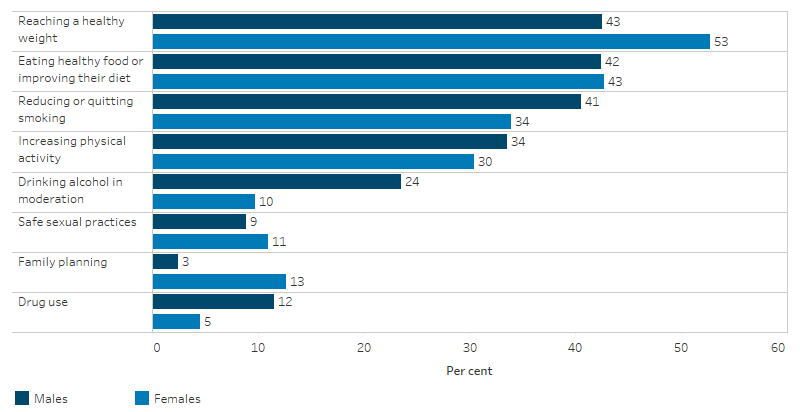
Source: Table D3.03.3. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
Indigenous Australians in the Northern Territory were less likely to have consulted a GP or specialist in the last 12 months than those living in other areas. The results were lowest in the Northern Territory (80%) and highest in Victoria (92%). The proportion of Indigenous Australians who discussed lifestyle issues with a GP or health professional in the last 12 months was lowest in the Northern Territory (36%) and highest in South Australia (57%) (Table D3.03.4).
By remoteness, the proportion of Indigenous Australians who consulted a GP or specialist in the last 12 months was lowest in Very remote areas (76%) and highest in Major cities (92%). Indigenous Australians who discussed lifestyle issues with a GP or health professional in the last 12 months was lowest in Very remote areas (32%) and highest in Major cities (51%) (Table D3.03.5, Figure 3.03.3).
Figure 3.03.3: Proportion of Indigenous Australians aged 15 and over who discussed lifestyle issues with a doctor or health professional in last 12 months, by remoteness, 2018–19
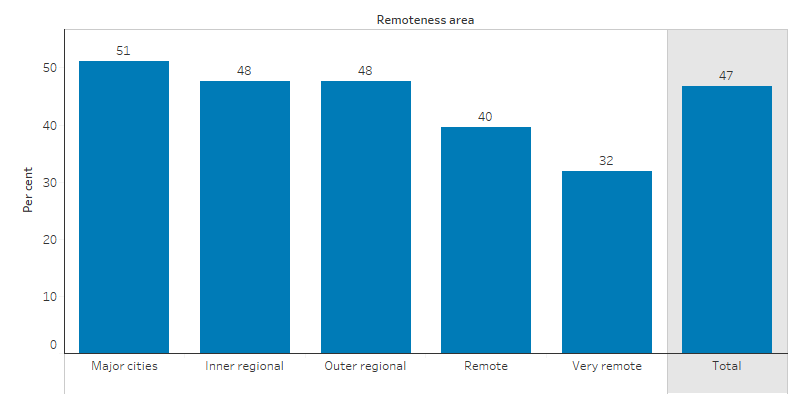
Source: Table D3.03.5. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
Health promotion issues discussed with a general practitioner
The Bettering the Evaluation and Care of Health (2010–2015) data showed that 32% of all clinical and therapeutic treatments provided by GPs to Indigenous patients related to health promotion. For Indigenous Australians, selected clinical treatments included general advice/education (57 per 1,000), advice/education treatment (40 per 1,000), counselling/advice for nutrition and weight (39 per 1,000) and counselling/advice for smoking (21 per 1,000).
After adjusting for differences in the age structure between the two populations, the rate at which GPs provided counselling and advice about smoking was 2.7 times as high for Indigenous patients (19 per 1,000) than Other patients (7 per 1,000). The rate was almost twice as high for Indigenous than Other patients for both alcohol (13 per 1,000 compared with 7 per 1,000) and lifestyle advice (7.4 per 1,000 compared with 4 per 1,000). (Other patients includes non-Indigenous patients and patients for whom Indigenous status was not stated.)
The rate of GP clinical treatments relating to health promotion was higher for Indigenous Australians (204 per 1,000 GP encounters) compared with Other Australians (178 per 1,000 GP encounters) (Table D3.03.6). Other Australians includes those who were non-Indigenous and those whose Indigenous status was not stated.
Indigenous primary health care organisation health promotion programs and activities
In 2017–18, all Commonwealth-funded Indigenous primary health care organisations provided a range of health promotion programs and activities. These included immunisation services to children and adults (86% and 84% of organisations, respectively), healthy lifestyle programs (provided by 79% of organisations), sexual health promotion (provided by 70% of organisations) and mental health promotion activities (provided by 55% of organisations) (Table D3.03.9, Figure 3.03.4).
Figure 3.03.4: Proportion of Indigenous primary health care organisations providing health promotion by type of program/activity, 2017–18
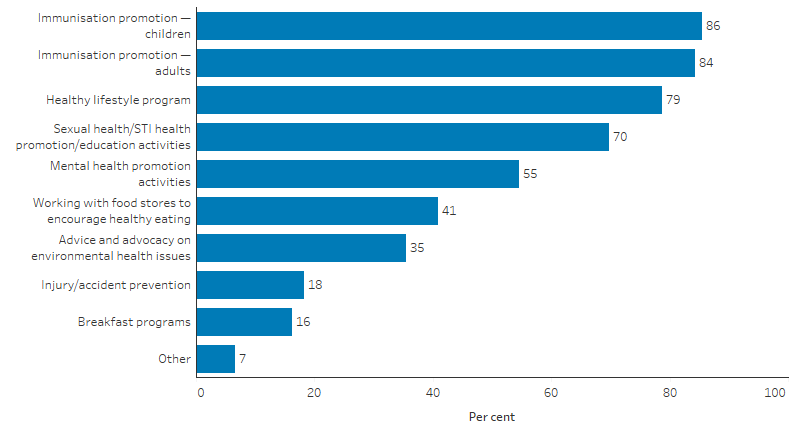
Source: Table D3.03.9. AIHW analyses of Online Services Report data collection, 2017–18.
Almost all (96%) of these organisations also provided group activities. These included the promotion of physical activity/healthy weight activities (70%), living skills (such as cooking and nutrition groups) (66%), substance-specific activities for tobacco (65%), alcohol treatment/prevention (38%) and maternal and baby/child health groups (49%) (Table D3.03.10).
Health promotion activities were a key feature of programs run by Indigenous Australian substance-specific services. These included the promotion of physical activity/healthy weight activities (80%), substance-specific activities for tobacco (67%) and alcohol treatment/prevention (80%), living skills groups (75%), men’s groups (80%) and women’s groups (77%) (Table D3.03.11).
Research and evaluation findings
Evidence on the effectiveness of health promotion is mixed across a range of settings and disease types with some approaches being more effective than others for different population groups (Davidson et al. 2014; Jackson & Waters 2005; Liu et al. 2012; Schloemer & Schröder-Bäck 2018). Approaches include adapting interventions to increase relevance, cultural acceptability and uptake. However, there is still insufficient evidence on the clinical effectiveness or cost-effectiveness of adapted interventions. Research highlights that more comparisons are needed between adapted and standard interventions (Liu et al. 2012).
A small study of urban Indigenous young people found no change in behaviours but some change in knowledge and attitudes following health promotion interventions in school (Malseed et al. 2014).
A recent small study of a remote Indigenous community in North-Eastern Arnhem Land highlighted that policy initiatives that address social and economic disadvantage are needed alongside community-led health promotion initiatives (Strate K 2020). The study followed a three-year period of community-led health promotion initiatives. It found that there may have been some benefits to chronic conditions risk factors, including stabilisation of body composition and increase in good HDL cholesterol. However, there were less favourable trends for diabetes and total cholesterol, and smoking rates remained high (Strate K 2020).
One study highlighted the need for a social determinants lens to be considered when planning and implementing Aboriginal health promotion programs (Vallesi et al. 2018).
A recent study in remote communities in Central Australia aimed to identify culturally-led behaviours and attitudes that present obstacles to the effectiveness of health promotion messages on trachoma prevention. These obstacles can hamper the responsiveness to guidance on facial cleanliness, for some people living in communities vulnerable to trachoma. The study suggested the following approaches: case management that encourages and supports individual families to focus on washing that is necessary for eye health; information campaigns that encourage people to separate the need for facial cleanliness from the way in which people prefer to present themselves; and engaging messages on trachoma prevention that focus on positive empowerment (Abbott 2020).
There is limited evaluation evidence on the effectiveness of Indigenous specific health promotion programs particularly in terms of lasting impact on health outcomes.
A literature review found that while Indigenous health promotion tools were widely available, only 15% had been evaluated, and only half of these evaluations were considered comprehensive (McCalman et al. 2014). From those comprehensive evaluations, programs that were found to be more successful had allowed local communities to determine the end product by asking them what type of health promotion they would like, on what topic and how they would like it delivered (Malseed et al. 2014; Schoen et al. 2010).
The Holman Review 2014 evaluated various aspects of Western Australian Aboriginal health interventions covering environmental health, smoking, nutrition, physical activity, healthy lifestyles, alcohol and drugs, maternal and child health, mental health, youth health and chronic disease. They were found to be innovative and outstanding value for money (Holman & Joyce 2014).
The Western Australian Government Strong Spirits, Strong Minds media campaign, aims to raise awareness of the harms associated with alcohol and other drug issues among Aboriginal people, families and communities in the Perth Metropolitan area. Evaluation results indicate that it is a highly effective and successful strategy. Aboriginal young people were more aware of how to obtain help from alcohol and other drug services after being exposed to the campaign (Mental Health Commission 2016).
Implications
Not all health campaigns are effective. Factors that influence health behaviour and health behaviour change among Indigenous Australians are complex and poorly understood (Waterworth et al. 2015). Social media may be a useful strategy to provide health messages and content among Indigenous Australians, but the effects on health need to be further investigated (Hefler et al. 2018; Walker et al. 2019). More research also needs to be undertaken into the usefulness and effectiveness of using a social determinants lens when planning and implementing Indigenous-specific health promotion programs.
While studies can model the continued effectiveness of health promotion interventions, there is limited evidence on long-term behavioural change (Merkur et al. 2013). More systematic research investigating the effectiveness of peer-led interventions is required, specifically for those directed at Indigenous Australians. To improve health outcomes for Indigenous youth, greater knowledge of the mechanisms and context under which peer-delivered health promotion is useful in comparison to other methods of health promotion is needed (Vujcich et al. 2018). At the heart of health promotion is effective communication that takes into account Aboriginal and Torres Strait Islander languages and culture to support people to live healthy lives (Vass et al. 2011).
Features of effective health promotion interventions for Indigenous communities include involving local Indigenous people in the design and implementation of programs; acknowledging different drivers that motivate individuals; building effective partnerships between community members and the organisations involved; cultural understanding and mechanisms for effective feedback to individuals and families; and developing trusting relationships, community ownership and support for interventions (Black 2007). Family-centred approaches across the life course have also been recommended in the prevention of chronic disease (Griew et al. 2007).
A recent review of evaluation methods and quality in Australian health promotion agencies highlighted the importance of improving the quality of evaluations in health promotion and preventative health to help build the evidence base for prevention strategies (Schwarzman et al. 2019).
The policy context is at Policies and strategies.
References
- Abbott T 2020. Who are you getting dolled up for? Cultural influences on the effectiveness of trachoma prevention programs in Aboriginal communities in Central Australia. Alice Springs.
- Black A 2007. Evidence of effective interventions to improve the social and environmental factors impacting on health: Informing the development of Indigenous Community Agreements. (ed., Department of Health and Ageing). Canberra: DoHA.
- Davidson EM, Liu JJ, Bhopal RS, White M, Johnson MR, Netto G et al. 2014. Consideration of ethnicity in guidelines and systematic reviews promoting lifestyle interventions: a thematic analysis. The European Journal of Public Health 24:508-13.
- Griew R, Tilton E, Stewart J, Eades S, Lea T, Peltola C et al. 2007. Family Centred Primary Health Care: review of evidence and models (ed., Office of Aboriginal and Torres Strait Islander Health, Department of Health and Ageing). Canberra: OATSIH.
- Hefler M, Kerrigan V, Henryks J, Freeman B & Thomas DP 2018. Social media and health information sharing among Australian Indigenous people. Health Promotion International.
- Holman C & Joyce S 2014. Promising Future: WA Aboriginal Health Programs. Review of performance with recommendations for consolidation and advance. Perth.
- Jackson N & Waters E 2005. Criteria for the systematic review of health promotion and public health interventions. Health Promotion International 20:367-74.
- Liu JJ, Davidson E, Bhopal RS, White M, Johnson MRD & Netto G 2012. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed-methods evidence synthesis. Health Technology Assessment 16.
- Malseed C, Nelson A & Ware R 2014. Evaluation of a school-based health education program for urban Indigenous young people in Australia. Health 6:587.
- McCalman J, Tsey K, Bainbridge R, Rowley K, Percival N, Lynette O et al. 2014. The characteristics, implementation and effects of Aboriginal and Torres Strait Islander health promotion tools: a systematic literature search. BMC Public Health 14:712.
- Mental Health Commission 2016. Strong Spirit Strong Mind metro project: campaign evaluation. Perth.
- Merkur S, Sassi F & McDaid D 2013. Promoting health, preventing disease: is there an economic case? Copenhagen: WHO.
- Schloemer T & Schröder-Bäck P 2018. Criteria for evaluating transferability of health interventions: a systematic review and thematic synthesis. Implementation science 13:88.
- Schoen D, Balchin D & Thompson S 2010. Health promotion resources for Aboriginal people: lessons learned from consultation and evaluation of diabetes foot care resources. Health Promotion Journal of Australia 21:64-9.
- Schwarzman J, Nau T, Bauman A, Gabbe BJ, Rissel C, Shilton T et al. 2019. An assessment of program evaluation methods and quality in Australian prevention agencies. Health Promotion Journal of Australia.
- Strate K BJ, Maple-Brown L, Garrngulkpuy J, Maypilama E, Scarlett M, O'Dea K, Barr EL 2020. Chronic condition risk factor change over time in a remote Indigenous community. Rural and Remote Health 20.
- Vallesi S, Wood L, Dimer L & Zada M 2018. “In Their Own Voice”—Incorporating Underlying Social Determinants into Aboriginal Health Promotion Programs. International journal of environmental research and public health 15:1514.
- Vass A, Mitchell A & Dhurrkay Y 2011. Health literacy and Australian Indigenous peoples: an analysis of the role of language and worldview. Health Promotion Journal of Australia 22:33-7.
- Vujcich D, Thomas J, Crawford K & Ward J 2018. Indigenous youth peer-led health promotion in Canada, New Zealand, Australia, and the United States: A systematic review of the approaches, study designs, and effectiveness. Frontiers in public health 6:31.
- Walker T, Palermo C & Klassen K 2019. Considering the Impact of Social Media on Contemporary Improvement of Australian Aboriginal Health: Scoping Review. JMIR public health and surveillance 5:e11573.
- Waterworth P, Pescud M, Braham R, Dimmock J & Rosenberg M 2015. Factors Influencing the Health Behaviour of Indigenous Australians: Perspectives from Support People. PloS one 10:e0142323.
- WHO (World Health Organization) 2008. The Bangkok charter for health promotion in a globalized world.

