Key messages
- In 2018–19, 13% (65,284) of Aboriginal and Torres Strait Islander adults reported having diabetes or high sugar levels. This increased with age, from 0.8% for those aged 18–24, to more than one-third of those aged 55 and over (36%).
- In 2018–19, 92% of Indigenous adults who reported having diabetes had their blood glucose checked in the last 12 months.
- Endocrine, nutritional and metabolic diseases, consisting largely of diabetes, was the 5th leading cause of death for Indigenous Australians in 2015–2019.
- In 2015–2019, 7.3% of deaths of Indigenous Australians were due to diabetes (1,124 deaths or 31 deaths per 100,000 population), with the rates being higher in remote (65 per 100,000) than non-remote areas (20 per 100,000).
- There were 8,953 hospitalisations of Indigenous Australians where the principal diagnosis was diabetes in 2017–19.
- From 2012–13 to 2018–19, based on age-standardised rates, hospitalisations with diabetes as a principal diagnosis increased by 15% for Indigenous Australians and 16% for non-Indigenous Australians
- Evidence suggests that children born to women with diabetes have increased risk of youth onset chronic disease including diabetes. The burden of diabetes in pregnant Indigenous women is amplified by the effect of social determinants of health.
- An evaluation of the Wurli Wurlinjang Health Service Diabetes Day Program at found that it resulted in an improvement in social and emotional wellbeing, and an increase in the number of people receiving medical check-ups.
- An evaluation of a school-based health promotion program called Deadly Choices found that it improved knowledge, attitudes and self-efficacy regarding chronic disease and risk factors among young Aboriginal and Torres Strait people. Significant increases were found in physical activity levels, breakfast frequency, fruit and vegetable consumption and in the uptake of health checks.
Why is it important?
Diabetes is a long-term chronic condition in which blood glucose levels become too high because the body produces little or no insulin, or cannot use insulin properly. Over many years, high blood glucose levels can damage various parts of the body, especially the heart and blood vessels, eyes, kidneys and nerves. It can result in permanent disability (such as blindness and lower limb amputations), mental health problems, reduced quality of life and premature death (AIHW 2015; Burrow & Ride 2016).
Aboriginal and Torres Strait Islander people have a higher rate of diabetes as well as a higher rate of hospitalisation and death from diabetes than non-Indigenous Australians.
There are three main types of diabetes:
- Type 2 diabetes—affected almost 1.2 million Australians (4.5% of the population) in 2020. Type 2 diabetes is a significant contributor to morbidity and mortality for Indigenous Australians. It is largely preventable and associated with lifestyle factors including physical inactivity, poor diet, being overweight or obese, excessive alcohol consumption and tobacco smoking (AIHW 2022b). Heredity, low birthweight and intra-uterine factors are also associated with increased risk (Burrow & Ride 2016). Type 2 diabetes can develop over a long period of time and initially may be managed with diet, exercise and lifestyle changes. However, as the disease progresses medications may be required, including taking insulin in order to manage blood glucose levels (Diabetes Australia 2020a).
- Type 1 diabetes—While there are no accurate national data on the total number of cases for all Australians, the National (insulin treated) Diabetes register (NDR) estimates that there were 13,000 children and young adults (aged between 0 and 19) living with type 1 diabetes in 2020 (AIHW 2022b). Type 1 diabetes is a lifelong autoimmune disease that usually has an onset in childhood or early adolescence and requires management with insulin to ensure that blood glucose levels remain within a safe range. It is not known what causes the autoimmune reaction that initiates type 1 diabetes. Type 1 diabetes is not linked to modifiable risk factors and it is not known how to prevent it (Diabetes Australia 2020b).
- Gestational diabetes—around 1 in 7 Australian females who gave birth in hospital were diagnosed with gestational diabetes (44,800) in 2019–20 (AIHW 2022b). The fastest growing type of diabetes nationally, gestational diabetes occurs during pregnancy and is usually resolved after the baby is born (Diabetes Australia 2020c). Gestational diabetes can be managed with a healthy diet and regular exercise, however in some instances women may require medication and/or insulin injections (Diabetes Australia 2020c). High blood glucose levels can cause complications for both the mother and baby during pregnancy, and gestational diabetes also increases the risk of developing type 2 diabetes for the mother.
Diabetes is a major public health problem worldwide, with global estimates indicating that the disease affects 415 million people and is increasing rapidly (Al-Lawati 2017). In 2013, 1 in 12 of global all-cause deaths were attributable to diabetes in adults (IDF Diabetes Atlas Group 2015). High rates of metabolic disease (including diabetes) are associated with rapid transitions in lifestyle among previously active populations. Indigenous populations with similar histories of European colonisation have been particularly impacted by epidemiological transitions (Hare et al. 2022; Harris et al. 2017). Diabetes lowers quality of life, increases medical expenses and significantly increases disease-related deaths (Shi 2016).
Burden of disease
In 2018, among Indigenous Australians, 7,966 years of healthy life (DALY) were lost due to endocrine disorders (largely diabetes), accounting for 3.3% of the total disease burden (AIHW 2022e).
Of the total burden attributed to endocrine disorders, 87% was due to type 2 diabetes, 7.5% due to type 1 diabetes, 3.1% due to other diabetes types (excluding gestational diabetes), and the remainder due to other endocrine disorders, such as thyroid disorders. Most of the burden due to endocrine disorders was non-fatal (57%) rather than fatal (43%).
The burden due to endocrine disorders was higher in more remote areas and in areas with greater socioeconomic disadvantage (based on 2016 Indigenous Relative Socioeconomic Outcomes index).
After adjusting for differences in the age structure between the two populations, the rate of burden due to endocrine disorders for Indigenous Australians was 3.6 times the rate for non-Indigenous Australians (16.2 and 4.5 DALY per 1,000 people, respectively). Endocrine disorders were responsible for 5.3% of the total gap between Indigenous and non-Indigenous Australians (AIHW 2022e).
Between 2003 and 2018, the burden due to endocrine disorders among Indigenous Australians decreased (by 13 DALY per 1,000 population, based on age-standardised rates), as did the gap in burden between Indigenous and non-Indigenous Australians (by 12 DALY per 1,000 population).
The aforementioned information on disease burden represents the direct impact of endocrine disorders. Diabetes is an important risk factor for other diseases such as coronary heart disease and chronic kidney disease. These indirect effects of diabetes are not included in the disease burden for endocrine disorders but are instead included in the disease group where the disease effects are more immediate—for these examples, in cardiovascular (circulatory) diseases, and kidney and urinary diseases, respectively. An estimate of the impact of diabetes on these other diseases can be seen through considering high blood plasma glucose as a risk factor. In 2018, among Indigenous Australians, high blood plasma glucose was responsible for 38% of the burden due to peripheral vascular disease, 25% of the chronic kidney disease burden, 14% of the coronary heart disease burden and 13% of the stroke burden (AIHW 2022f).
Data findings
Deaths from diabetes
Deaths data in this measure are from five jurisdictions for which the quality of Indigenous identification is considered to be adequate: New South Wales, Queensland, Western Australia, South Australia and the Northern Territory. Data by remoteness are reported for all jurisdictions combined (see Data sources: National Mortality Database).
In the 5-year period between 2015–2019, 7.3% (1,124) of total deaths of Indigenous Australians were due to diabetes. The proportion of total deaths due to diabetes was higher for Indigenous females (608 deaths or 8.7% of all Indigenous female deaths) than Indigenous males (516 or 6.1%).
In 2015–2019, the rate of death due to diabetes among Indigenous Australians was 31 deaths per 100,000 population. The rate was:
- higher for females than males (34 compared with 29 deaths per 100,000 population).
- lowest in New South Wales (17 per 100,000) and highest in the Northern Territory (68 per 100,000)
- lower in non-remote areas (Major cities, Inner regional and Outer regional combined) (20 per 100,000) than in remote areas (Remote and Very remote combined) (65 per 100,000) (Table D1.23.2, D1.23.30, D1.23.32).
After adjusting for differences in the age structure between the two populations, the rate of deaths due to diabetes for Indigenous Australians was 4.7 times the rate for non‑Indigenous Australians. The difference was larger in remote areas, where the rate for Indigenous Australians was 8.8 times the rate for non-Indigenous Australians (compared with 3.0 times as high in non-remote areas) (Table D1.23.30).
Endocrine, nutritional and metabolic diseases (largely diabetes) was the 5th leading cause of death for Indigenous Australians in 2015–2019, accounting for 8.6% of Indigenous deaths.
Deaths due to endocrine, nutritional and metabolic diseases (largely diabetes) was the third leading cause of the gap in death rates between Indigenous and non‑Indigenous Australians (17% of the total gap in death rates), after cardiovascular (circulatory) diseases (21%) and cancer and other neoplasms (18%) (Table D1.23.1).
Among Indigenous Australians in the 2015–2019 period, the leading cause of death due to diabetes was type 2 diabetes (662 or 59% of all diabetes deaths), followed by other specified and unspecified diabetes (418 or 37%) and type 1 diabetes (44 or 3.9%) (Table D1.23.32).
Diabetes does not often lead directly to death, rather it contributes to deaths from other causes (for example, cardiovascular (circulatory) disease or kidney disease). This is referred to as associated cause of deaths (AIHW 2017). In 2015–2019, there were 2,989 deaths of Indigenous Australians in which diabetes was listed as an underlying or associated cause of death (defined as multiple causes of death) (see Box 1.09.1). Therefore, 19% of the total deaths of Indigenous Australians was partly due to diabetes (Table D1.23.24).
Hospitalisation for diabetes
Between July 2017 and June 2019, there were 8,953 hospitalisations of Indigenous Australians with a principal diagnosis of diabetes, representing 0.8% of all hospitalisations for Indigenous Australians. This corresponds to a rate of 5.4 hospitalisations per 1,000 population, with a higher rate for Indigenous females than males (6.2 and 4.5 per 1,000, respectively) (Table D1.09.10).
Of these 8,953 hospitalisations with a principal diagnosis of diabetes, 1,291 hospitalisations (14%) were for diabetes in pregnancy (consisting of pre-existing type 1 and type 2 diabetes (6%) and gestational diabetes (8%)). The remaining 7,664 hospitalisations were for type 2 diabetes (60%) and type 1 diabetes (24%) (Table D1.09.10).
Excluding diabetes in pregnancy, hospitalisation rates were similar for Indigenous males and females (4.5 and 4.7 per 1,000, respectively) (Table D1.09.7). Hospitalisation rates for diabetes increased with age, increasing from 0.3 hospitalisations per 1,000 population for Indigenous Australians aged 0–4 to 18 per 1,000 for those aged 65 and over. Rates were higher for Indigenous females than Indigenous males until the 45–54 age group, when the rate for males began to increase more sharply than the rate for females (Table 1.09.7, Figure 1.09.1).
Figure 1.09.1: Hospitalisation rates for diabetes (based on principal diagnosis), by Indigenous status and age, Australia, July 2017 to June 2019
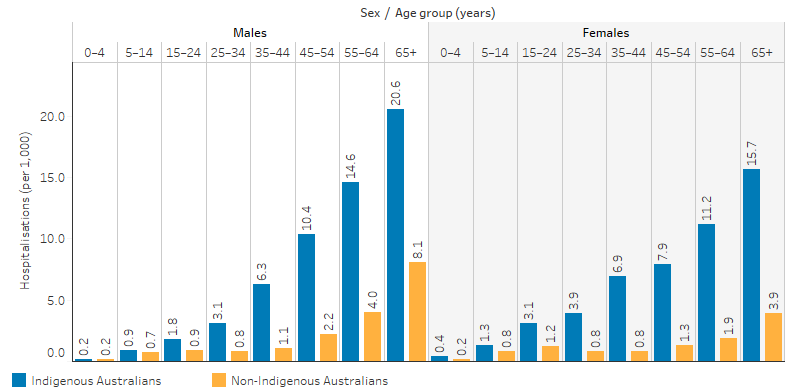
Note: Excludes diabetes during pregnancy.
Source: Table D1.09.7. AIHW analysis of National Hospital Morbidity Database.
Across all age groups, the relative difference in rates between Indigenous and non-Indigenous Australians were highest for those aged 35–44. Indigenous males aged 35–44 were 5.7 times as likely as non-Indigenous males of the same age group to be hospitalised for diabetes (6.3 and 1.1 hospitalisations per 1,000 population, respectively, excludes diabetes during pregnancy). Indigenous females aged 35–44 were 8.9 times as likely as non-Indigenous females of the same age group to be hospitalised for diabetes (6.9 and 0.8 per 1,000, respectively, excludes diabetes during pregnancy) (Table D1.09.7, Figure 1.09.1).
After adjusting for differences in the age structure between the two populations, the rate of hospitalisation for a principal diagnosis of diabetes for Indigenous Australians (excluding diabetes during pregnancy) was 3.8 times the rate of non-Indigenous Australians (Table D1.09.8).
From July 2017 to June 2019, the rate of hospitalisation for diabetes (excluding diabetes during pregnancy) was higher for Indigenous Australians living in remote than non-remote areas. The rate was highest for Indigenous Australians living in Remote areas (7.9 hospitalisations per 1,000 population), followed by Very remote areas (6.8 per 1,000). The rate was lowest in Major cities (3.3 per 1,000) (Table D1.09.9, Figure 1.09.2). The rate for Indigenous Australians also varied by jurisdiction, with the lowest rate in Tasmania (3.1 per 1,000) and highest in Western Australia (5.7 per 1,000) (Table D1.09.8).
Figure 1.09.2: Hospitalisation rates for diabetes (based on principal diagnosis) among Indigenous Australians, by remoteness, Australia, July 2017 to June 2019
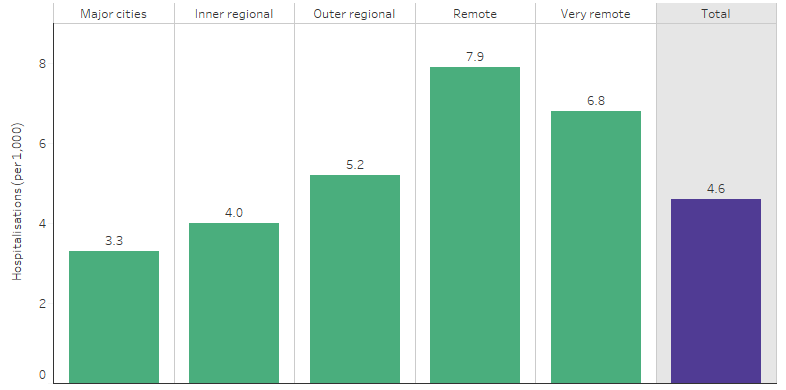
Note: Excludes diabetes during pregnancy.
Source: Table D1.09.9. AIHW analysis of National Hospital Morbidity Database.
From July 2017 to June 2019, there were 157,282 hospitalisations among Indigenous Australians where diabetes was recorded as a principal or additional diagnosis (this included hospitalisations with multiple causes and those where diabetes was not the main diagnosis) (Table D1.09.12).
Complications of diabetes such as lower limb amputations were also more common among Indigenous Australians than non-Indigenous Australians. A retrospective 2011–2013 analysis of those attending the High Risk Foot Clinic at the Townsville Hospital found that lower limb amputation occurred more commonly among Indigenous Australians (57%) compared with non-Indigenous Australians (29%), and that Indigenous status was associated as a risk factor for this outcome (OR 3.4) (Burrow & Ride 2016; Rodrigues et al. 2016).
Diabetes managed by general practitioners
Diabetes is a complex chronic disease that requires lifestyle modification and self-management. General practitioners (GPs) play a critical role of providing guidance for their patients in monitoring risk factors and medication management.
The Bettering the Evaluation and Care of Health Survey data (2010–15) showed that 5.5% of all problems managed by GPs for Indigenous patients were for diabetes. Type 2 diabetes accounted for 92% of all diabetes problems managed by a GP (82 per 1,000 encounters). After adjusting for differences in the age structure between the two populations, GPs managed diabetes for Indigenous Australians at 2.9 times the rate for Other Australians (non-Indigenous Australians and those with unknown/not stated Indigenous status) (Table D1.09.6).
MedicineInsight is a database managed by NPS MedicineWise containing data on care provided in general practice from over 700 Australian general practices. In 2020–21, MedicineInsight collected data from 471 general practices and 4,110 GPs (5.8% of all Australian general practices and 10.8% of all Australian GPs) (NPS MedicineWise 2022). Data from participating MedicineInsight general practices shows that type 2 diabetes (including diabetes type not specified) was among the top 10 conditions ever recorded for Indigenous Australians, with 7.3% of patients having a type 2 diabetes (or type not specified) diagnosis listed on their medical record. Of the 65,262 Indigenous patients who visited participating practices in 2020–21, type 2 diabetes (or type not specified) was the 7th most common condition recorded, with 3.7% of patients being recently diagnosed. When GPs were providing care to Indigenous Australians in 2020–21, on average:
- 8.7 per 100 clinical encounters were with a patient who had a recent diagnosis of type 2 diabetes (or type not specified)
- 16 per 100 clinical encounters were with a patient who had ever been diagnosed with type 2 diabetes (or type not specified).
Findings from ABS survey data
According to data from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS), around 8% of Indigenous Australians were living with diabetes (ABS 2019). This included Indigenous Australians of all ages and is not age-standardised. However, to better understand and capture the health risk to the Indigenous Australian population and to understand the disparity with the non-Indigenous Australian population, the following rates focus on those aged 18 and over (due to low rates occurring among children) and include those with high sugar levels. The age-specific rates have not been age-standardised.
The 2018–19 NATSIHS showed that 13% (65,284) of Indigenous Australians aged 18 and over reported having diabetes or high blood/urine sugar levels (HSL) (Table D1.09.14). After adjusting for differences in the age structure, Indigenous Australians were 2.8 times as likely to report having diabetes or HSL as non-Indigenous Australians—17% compared with 6%, respectively. Indigenous male adults reported having diabetes or HSL at a similar rate to Indigenous female adults (18% and 17%, respectively). Indigenous adults in remote areas reported a higher rate of diabetes or HSL (24%) than those in non-remote areas (15%). The rate of reported diabetes or HSL for Indigenous adults varied by states and territories, ranging from 9% in Tasmania to 24% in Western Australia (Table D1.09.2, Figure 1.09.3).
Figure 1.09.3: Age-standardised proportion of persons aged 18 and over who reported having diabetes or high sugar levels, by Indigenous status and state and territory, 2018–19
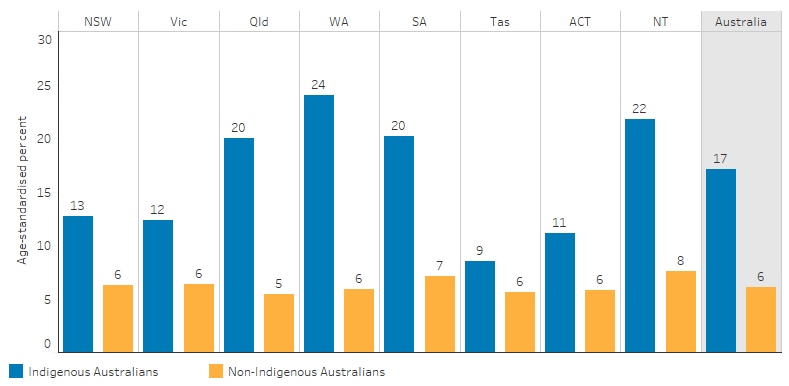
Source: Table D1.09.2. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19 and National Health Survey 2017–18.
Diabetes or HSL increased with age for Indigenous adults, from 0.8% for those aged 18–24, to more than one-third of those aged 55 and over (36%) (Table D1.09.2, Figure 1.09.4).
Figure 1.09.4: Proportion of adults who reported having diabetes or high sugar levels, by Indigenous status and age, 2018–19
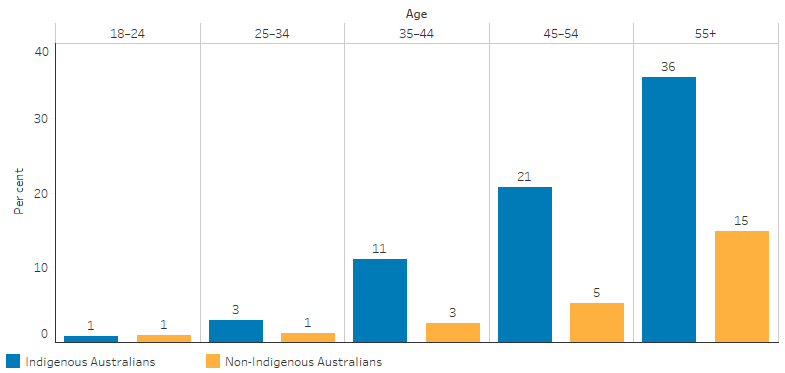
Source: Table D1.09.2. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19 and National Health Survey 2017–18.
Indigenous adults were more likely to report having diabetes or HSL if they:
- had completed Year 9 or below (3.3 times) compared with those who had completed Year 12.
- reported having fair/poor health status (2.8 times) compared with those who reported excellent/very good/good health status.
- were obese (1.8 times) compared with those who were not obese.
- reported having heart or cardiovascular (circulatory) problems (4.2 times) compared with those who did not.
- reported having kidney disease (3.6 times) compared with those who did not.
- had measured high blood pressure (1.8 times) compared with those who did not (Table D1.09.5).
In 2018–19, the main health actions taken by Indigenous Australians reporting diabetes or HSL were:
- 92% had their blood glucose checked in the last 12 months.
- 70% had taken lifestyle action relating to diet, weight loss and exercise in the last two weeks.
- 73% had a blood test (HbA1c) to manage diabetes in the last 12 months.
- 70% had their feet checked in the last 12 months.
- 62% used medicine/tablets in the last two weeks.
- 31% had been tested for diabetes/high sugar levels in the last three years.
- 24% had used insulin in the last two weeks (Table D1.09.4).
Diabetes data by type
Data on Indigenous Australians with type 2 diabetes are incomplete. National data on diabetes prevalence are primarily based on ABS health surveys as described earlier. However, data from the National Aboriginal and Torres Strait Islander Health Survey do not differentiate between type 1 and type 2 diabetes and excludes gestational diabetes.
Another source of data on the incidence of diabetes by type is the National (insulin-treated) Diabetes Register (NDR). However, not all Indigenous Australians with type 2 diabetes are registered with the National Diabetes Services Scheme (NDSS), and not all are insulin dependent. The NDR draws upon the NDSS as the source population for calculating incidence rates (new cases) of insulin-treated type 2 diabetes. This means rates of type 2 diabetes for Indigenous Australians (insulin or non-insulin dependent) are underestimated from both the NDR and NDSS (AIHW 2022a). This is a data gap, therefore, only information on the incidence of type 1 diabetes is presented below.
Type 1 diabetes
In 2020, there were 164 Indigenous Australians diagnosed with type 1 diabetes (19 cases per 100,000 population). After adjusting for differences in the age structures between the two populations, the incidence rates of type 1 diabetes for Indigenous Australians was 1.4 times the rate for non-Indigenous Australians (AIHW 2022a).
Gestational diabetes
The primary national data sources for gestational diabetes for Indigenous women are the National Hospital Morbidity Database and the National Perinatal Data Collection (AIHW 2019).
In 2019–20, there were around 1,900 new cases of gestational diabetes among Indigenous women, equating to 13% of Indigenous women aged 15–49 who gave birth in hospital. Incidence increased with age, peaking in the 45–49 age group at 33%; women in this age group were 5.2 times as likely to be diagnosed with gestational diabetes as Indigenous women aged 15–19 (6.4%).
After adjusting for differences in the age structure between the two populations, the incidence of gestational diabetes for Indigenous Australian women was around 1.1 times the rate for non-Indigenous women (AIHW 2022d).
Data from the National Perinatal Data Collection in 2019 showed that 12% of Indigenous women who gave birth had gestational diabetes and 2% had pre-existing diabetes. After adjusting for differences in the age structure between the two populations, Indigenous women who gave birth had gestational diabetes at 1.3 times the rate of non-Indigenous mothers, and had pre-existing diabetes at 4.1 times the rate of non-Indigenous mothers (Table D2.21.12).
Changes over time in deaths from diabetes
Between 2006 and 2019, the age-standardised rate of death due to diabetes decreased by 20% for Indigenous Australians, while the rate for non-Indigenous Australians did not change significantly. This resulted in a significant narrowing of the gap by 24%. However, over the decade 2010 to 2019, the rate of death due to diabetes for Indigenous Australians did not change significantly, nor did the rate for non-Indigenous Australians. The gap in the rates between the two populations also remained the same (Table D1.23.22, Figure 1.09.5).
Figure 1.09.5: Age-standardised death rates and changes in the gap due to diabetes, by Indigenous status, NSW, Qld, WA, SA and NT, 2006–2019
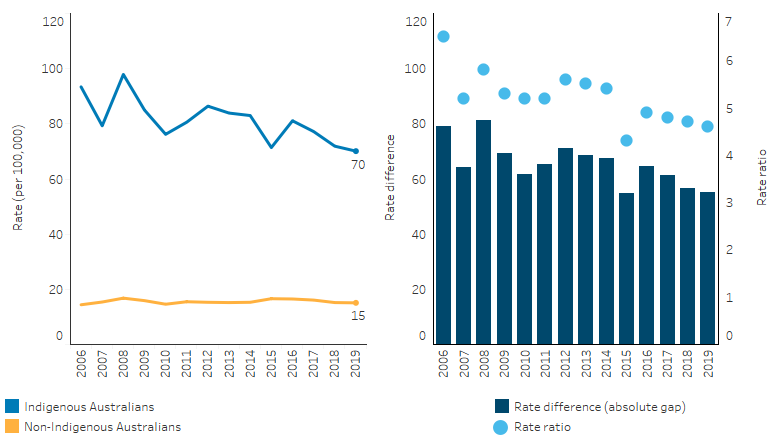
Note: Rate difference is the age-standardised rate (per 100,000) for Indigenous Australians minus the age-standardised rate (per 100,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D1.23.22. AIHW National Mortality Database.
Changes over time in hospitalisations for diabetes
From 2012–13 to 2018–19, the number of hospitalisations for Indigenous Australians with diabetes as the principal diagnosis increased from 2,749 to 4,087. After adjusting for differences in the age structure between the two populations, the rate of hospitalisation due to diabetes for Indigenous Australians increased by 15% and 16% for non-Indigenous Australians. The rate for Indigenous Australians was 3.7 times the rate for non-Indigenous Australians in 2012–13, and 3.8 times the non-Indigenous rate in 2018–19 (Table D1.09.12, Figure 1.09.6).
Figure 1.09.6: Age-standardised hospitalisation rates and changes in the gap for a principal diagnosis of diabetes, by Indigenous status, Australia, 2012–13 to 2018–19
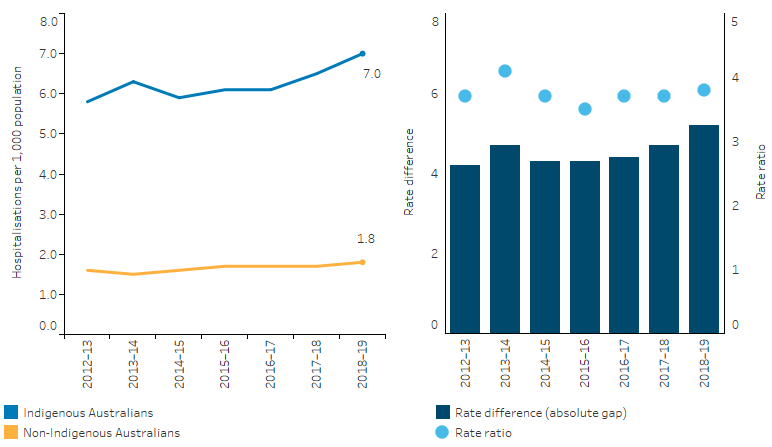
Note: Rate difference is the age-standardised rate (per 1,000) for Indigenous Australians minus the age-standardised rate (per 1,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D1.09.12. AIHW analysis of National Hospital Morbidity Database.
Where diabetes was recorded as a principal diagnosis or additional diagnosis, the number of hospitalisations among Indigenous Australians increased from 43,965 to 83,503 from 2012–13 to 2018–19. The age-standardised rate for Indigenous Australians increased by 50% over this period, compared with 24% for non-Indigenous Australians. The rate ratio for Indigenous Australians ranged between 3.5 (in 2014–15 and 2015–16) and 4.4 (in 2018–19) (Table D1.09.12).
Research and evaluation findings
Nationally, Indigenous Australians reported having diabetes or high sugar levels at a rate almost 3 times as high as non-Indigenous Australians. Research has shown that prevalence varies across regions, with studies of some individual communities having reported diabetes prevalence ranging from 3.5 to 33.1% (Burrow & Ride 2016; Minges et al. 2011; Shaw & Tanamas 2012).
The onset of diabetes occurs earlier among Indigenous Australians compared with non-Indigenous Australians, which leads to a greater burden of illness associated with the complications of diabetes, including kidney damage, loss of vision, peripheral nerve damage and peripheral vascular diseases (AIHW 2022e; Shaw & Tanamas 2012). Greater disease severity, lower access to health services and increased risk factors have also contributed to increased diabetes-related complications in Indigenous populations worldwide (Harris et al. 2017). Diabetes in pregnancy is also considered a key predictor and contributor to the increased prevalence of type 2 diabetes in Indigenous populations globally, with an increasing prevalence of gestational diabetes among Indigenous women leading to a cycle of intergenerational risk transmission (Harris et al. 2017; Ma & Popkin 2017).
Research has explored the increasing rate of type 2 diabetes among Indigenous Australian children. In 2006–11, Indigenous Australian children aged 10–14 were 8 times as likely to have type 2 diabetes as non-Indigenous children (AIHW 2014). Between 1990 and 2012 in Western Australia, the mean incidence of type 2 diabetes in Indigenous children was 21 times the rate of non-Indigenous children (Haynes et al. 2016). Titmuss and colleagues (2019) highlighted that Indigenous Australian young people with type 2 diabetes also have high rates of comorbidities which will have a significant effect on the burden of disease into the future, possibly leading to renal, cardiac, neurological and ophthalmological complications (Titmuss et al. 2019). In young Indigenous Australians with type 2 diabetes, 59% also have hypertension, 24% having dyslipidaemia and 61% having obesity (Haynes et al. 2016; Titmuss et al. 2019).
More broadly, higher rates of type 2/pre-existing diabetes and gestational diabetes among Indigenous mothers contribute to poorer pregnancy outcomes and long-term consequences for mothers and children. This can be seen among Indigenous women in countries with similar histories of colonisation such as Australia, Canada, New Zealand and the United States (Voaklander et al. 2020). Research suggests that prevention or delay of onset of type 2 diabetes in younger women is vital to improving pregnancy outcomes (Maple-Brown Louise et al. 2019). Evidence suggests that children born to women with diabetes have increased risk of youth onset chronic disease including diabetes. There may be an intergenerational effect contributing to the global epidemic of diabetes, with epigenetics potentially being a factor. The burden of diabetes facing pregnant Indigenous women is amplified by the effect of social determinants which makes it all the more important that services for diabetes care are culturally safe (Maple-Brown Louise J & Hampton 2020). Remoteness can be a compounding factor for Indigenous mothers with diabetes during pregnancy with a greater likelihood of poorer pregnancy outcomes (Duong et al. 2015).
The rate of Indigenous Australians with diabetes is higher in remote areas and they are also at greater risk of complications, for example kidney failure (Minges et al. 2011; Shaw & Tanamas 2012). The underlying causes are multifaceted. Firstly, diabetes is a chronic condition that requires complex medical care and often involves multiple healthcare providers. An observational study of remote Indigenous patients with diabetes in the Northern Territory has found patients who had adequate levels of access to primary healthcare had better diabetes management and lower level of hospitalisations, compared with those with fewer primary healthcare visits (Zhao et al. 2015). With less health service options available, self-management of diabetes is more necessary for remote residents than others who live in urban areas (Sav et al. 2015). However, living remotely poses barriers to accessing diabetes education resources. Moreover, people living in rural and remote areas are less likely to have completed Year 12 or equivalent education, have fewer employment opportunities, and have lower incomes while bearing higher costs for goods and services than urban residents (AIHW 2022g).
Poor diabetes management induces a high cost to the health system. In 2018–19, an estimated $3.0 billion of expenditure in the Australian health system was attributed to diabetes, representing 2.3% of the total disease expenditure. Medications dispensed through the Pharmaceutical Benefits Scheme (PBS) was the single highest area of diabetes expenditure ($776.8 million), followed by public hospital admitted patients ($604.8 million) and dental services ($513.8 million) (AIHW 2022b)
Health expenditure attributable to diabetes may be underestimated due to indirect costs, such as those significant costs associated with carers, annual lost wages, as well as the present and future effect of lost opportunities due to diabetes related morbidity, disability and premature mortality (Shaw & Tanamas 2012). A study into the cost effectiveness of primary health care for Indigenous Australians with diabetes in remote communities in the Northern Territory found that the cost of preventing one hospitalisation for diabetes was $248 for those in the medium-use of care group (patients who used primary care 2-11 times annually) and $739 for those in the high-use group (patients who used primary care 12 or more times annually). This is a substantial saving compared with the average cost of one hospitalisation ($2,915) (Thomas 2014).Due to the unique health characteristics and needs of Indigenous Australians, the National Aboriginal Community Controlled Health Organisation (NACCHO) was initiated to supplement mainstream health services to effectively engage and support Indigenous communities. The NACCHO represents hundreds of primary health care services across Australia that are initiated and operated by local Aboriginal and Torres Strait Islander communities, delivering holistic, comprehensive and culturally competent services.
Operated by the ACCHO Wurli-Wurlinjang Aboriginal Health Service, the Wurli Wurlinjang Diabetes Day Program commenced in 2008 with the aims of improving the wellbeing of Indigenous patients with type 2 diabetes through a supportive environment that promoted self-management and provided comprehensive care in Katherine, Northern Territory. The program considerably improved the social and emotional wellbeing of Indigenous Australians with type 2 diabetes. The program has also encouraged health seeking behaviour, which saw an increase in the number of people receiving medical check-ups and a small but significant improvement in clinical outcomes including better control of blood sugar, blood pressure and cholesterol (Entwistle et al. 2011).
Deadly Choices is a school-based health promotion and education program in Queensland aimed at improving knowledge, attitudes, self-efficacy, and behaviours of urban Indigenous young people regarding chronic disease and associated risk factors. Deadly Choices also encourages people to access their local Aboriginal Community Controlled Health Service to complete an annual health check. The program was established by the Institute of Urban Indigenous Health (IHUI), a Community Controlled Health Service. Deadly Choices also encourages people to access their local Aboriginal Community Controlled Health Service to complete an annual health check. An evaluation showed the program successfully improved knowledge, attitudes and self-efficacy regarding chronic disease and risk factors. Significant increases were found in physical activity levels, breakfast frequency, fruit and vegetable consumption and in the uptake of Aboriginal and Torres Strait Islander Health Checks (Medicare Item 715) (Malseed et al. 2014).
Aunty Jean’s Good Health Team began as a pilot project, with the idea that the community could work together to achieve better health outcomes. The main aim of the project was to develop a combined model of health promotion, education and self-management to support the development of good health behaviours and strategies for Indigenous Australians with chronic and complex care requirements. Led by Elders, the program ran for 12 weeks in the Illawarra region of New South Wales and involved completing 12 modules and a self-managed home program activity. Evaluation of the project showed improvements in self-management, the development of appropriate and effective working partnerships, culturally acceptable and appropriate information sharing and enhanced capacity in physical activity and self-management strategies. The evaluation also indicated improved health measures such as blood pressure and blood glucose levels. Essential factors contributing to the success of the program include leadership from Elders, strong existing relationships within the community and between the community and health professionals, and the location of the program within a safe community space (Curtis et al. 2004).
Implications
Reducing the burden of disease for Indigenous Australians due to diabetes and the substantial associated public and social health costs, requires significant effort across the life course, generations, and the health care continuum, beginning with preconception and pregnancy.
Policies and interventions should include a focus on primary prevention that aims to stop the development, or delay the onset, of type 2 diabetes (for example, through a healthy diet and lifestyle and physical activity) (Burrow & Ride 2016; Shaw & Tanamas 2012). Implementing strategies to achieve effective secondary prevention to stop the development of diabetes-related complications through lifestyle changes and medication is also crucial.
As there is no mechanism for preventing type 1 diabetes, further research on finding a cure for this disease and on improved treatments is needed (Shaw & Tanamas 2012). Further research into whether type 1 diabetes incidence is increasing for Indigenous Australians, or whether the trend is more reflective of data volatility or increased detection, is also worth exploring.
Primary health care has an essential role in assessing diabetes risk, and the prevention, detection, and management of diabetes. The Aboriginal and Torres Strait Islander Health Check (Medicare Item 715) is a screening tool used in primary health care to aid in the early detection of chronic diseases such as diabetes among Indigenous Australians. Through this health check patients can have their risk of developing diabetes over the next five years assessed using the Australian type 2 diabetes risk assessment tool. Patients identified as high risk can be referred to a lifestyle modification program and other appropriate prevention strategies and interventions can be recommended. However, once diagnosed, diabetes requires ongoing management in primary health care to help patients managing blood sugar levels and other effects of the disease. Other Medicare items coordinate complex and multidisciplinary diabetes care (see measure 3.05 Chronic disease management). There are also government programs designed to improve Indigenous Australians’ access to medicines to improve compliance with medication and reduce barriers such as the cost of the medications and access to pharmacies.
It is crucial that Indigenous Australians with diabetes have access to appropriate diabetes support, education and services and that the workforce across the health sector has the capability to deliver evidence-based diabetes care (Department of Health 2021). Culturally safe and competent health care is particularly important for Indigenous Australians managing a complex chronic disease such as diabetes.
The high levels of diabetes among Indigenous Australians reflect a broad range of historical, social and cultural factors. This presents specific challenges in the management and prevention of diabetes including in providing access to effective care services that are tailored to community needs and that are culturally appropriate (Burrow & Ride 2016). This highlights the major role of Aboriginal Community Controlled Health Services in delivering culturally safe health care to Indigenous Australians including community level health promotion, diabetes prevention, risk assessment and ongoing diabetes management.
Indigenous Australians living in remote areas face barriers to accessing health care, including specialist care, and diabetes education resources; this brings greater risk of diabetes complications. Indigenous Australians living in remote areas have higher prevalence of diabetes and higher rates of hospitalisations and death from diabetes. This indicates the unmet need for appropriate and adequately resourced diabetes prevention and management through primary health care in these locations.
The National Diabetes Services Scheme (NDSS) provides subsidised products and support services to help people in managing diabetes. However, many Indigenous Australians with diabetes have not registered with the NDSS. Where Indigenous Australians live in remote and very remote locations, NDSS Access Points may be limited, but patients may be obtaining diabetes-related products or services through other targeted Indigenous-specific programs (AIHW 2022c). Efforts to encourage Indigenous Australians with diabetes to register will yield benefits for patients and improve the coverage and quality of the data.
Research has showed that during 2020 many Aboriginal and Torres Strait Islander people disengaged from their routine diabetes and health care management plans due to social distancing, fear of exposure to COVID-19, and a focus on other priorities. In 2021 the NDSS launched a campaign, Back on Track, to encourage Indigenous Australians with type 2 diabetes to reengage with their diabetes healthcare teams and their diabetes management after the significant disruptions caused by COVID-19.
The National Aboriginal and Torres Strait Islander Health Plan 2021-2031 (the Health Plan), released in December 2021, is the overarching policy framework to drive progress against the Closing the Gap health targets and priority reforms. Implementation of the Health Plan aims to drive structural reform towards models of care that are prevention and early intervention focused, with greater integration of care systems and pathways across primary, secondary and tertiary care. It also emphasises the need for mainstream services to address racism and provide culturally safe and responsive care, and be accountable to Aboriginal and Torres Strait Islander people and communities. The Health Plan emphasises that action to address cardiovascular disease, diabetes, ear, eye and renal health, and rheumatic heart disease, remain key priorities.
Measure 3.05 Chronic disease management, provides more information on the effectiveness of the health system in providing diabetes care, including on the need for regular monitoring of blood glucose levels for patients with diabetes. Commonwealth-funded Indigenous primary health care organisations provide national Key Performance Indicators data on a range of process of care measures including regular testing of blood glucose levels for patients with diabetes. This information helps with the continuous quality improvement of services and serves as a useful example to other primary care services about the regular and ongoing care needs of patients with diabetes.
The policy context is at Policies and strategies.
References
- ABS (Australian Bureau of Statistics) 2019. National Aboriginal and Torres Strait Islander Health Survey, 2018-19. Vol. Cat No. 4715.0. Canberra: ABS.
-
ABS 2019. National Aboriginal and Torres Strait Islander Health Survey, 2018-19. Vol. Cat No. 4715.0. Canberra: ABS.
-
AIHW (Australian Institute of Health and Welfare) 2014. Type 2 diabetes in Australia’s children and young people: a working paper. Diabetes Series no. 21. Cat. no. CVD 64. Canberra: AIHW.
-
AIHW 2015. Cardiovascular disease, diabetes and chronic kidney disease—Australian facts: Aboriginal and Torres Strait Islander people. Canberra: AIHW.
-
AIHW 2017. Deaths among people with diabetes in Australia, 2009–2014. Cat. no. CVD 79. Canberra: AIHW.
-
AIHW 2019. Improving national reporting on diabetes in pregnancy: technical report. Cat. no. CDK 13. Canberra: AIHW.
-
AIHW 2021. Deaths in Australia. Canberra: AIHW.
-
AIHW 2022a. Incidence of insulin-treated diabetes in Australia. Canberra: AIHW. Viewed 28 July 2022.
-
AIHW 2022b. Diabetes: Australian facts. Canberra: AIHW. Viewed 28/09/2022.
-
AIHW 2022c. The National (insulin-treated) Diabetes Register 2020; Quality Statement. Canberra: AIHW. Viewed 29/8/2022.
-
AIHW 2022d. Diabetes: Australian facts, Gestational diabetes. Canberra: AIHW. Viewed 28 July 2022.
-
AIHW 2022e. Australian Burden of Disease Study: Impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018. Canberra: Australian Institute of Health and Welfare.
-
AIHW 2022f. Australian Burden of Disease Study 2018: Interactive data on risk factor burden among Aboriginal and Torres Strait Islander people. AIHW. Viewed May 2022.
-
AIHW 2022g. Rural and remote health. Viewed 29/08/2022.
-
Al-Lawati JA 2017. Diabetes mellitus: a local and global public health emergency! Oman medical journal 32:177.
-
Burrow S & Ride K 2016. Review of diabetes among Aboriginal and Torres Strait Islander people. Australian Indigenous HealthInfoNet No.17.
-
Curtis S, Pegg D & Curtis O 2004. Aunty Jean's Good Health Team: listening to the voices of the Elders to create an Aboriginal chronic and complex care program. Wollongong: Illawarra Health.
-
Department of Health 2021. Australian National Diabetes Strategy 2021-2030. Canberra: Department of Health.
-
Diabetes Australia 2020a. Type 2 diabetes. Viewed June 2020.
-
Diabetes Australia 2020b. What is diabetes. Viewed December 2019.
-
Diabetes Australia 2020c. Gestational diabetes. Viewed September 2020.
-
Duong V, Davis B & Falhammar H 2015. Pregnancy and neonatal outcomes in Indigenous Australians with diabetes in pregnancy. World journal of diabetes 6:880.
-
Entwistle P, Entwistle D & Stothers K 2011. Wurli-Wurlinjang Diabetes Day Program: evaluation report. Katherine, NT: Centre for Remote Health, Flinders University and Charles Darwin University.
-
Hare MJL, Zhao Y, Guthridge S, Burgess P, Barr E, Ellis E et al. 2022. Prevalence and incidence of diabetes among Aboriginal people in remote communities of the Northern Territory, Australia: a retrospective, longitudinal data-linkage study. BMJ Open 5.
-
Harris SB, Tompkins JW & TeHiwi B 2017. Call to action: a new path for improving diabetes care for Indigenous peoples, a global review. Diabetes research and clinical practice 123:120-33.
-
Haynes A, Kalic R, Cooper M, Hewitt JK & Davis EA 2016. Increasing incidence of type 2 diabetes in Indigenous and non-Indigenous children in Western Australia, 1990-2012. The Medical Journal of Australia 204:303.
-
IDF Diabetes Atlas Group 2015. Update of mortality attributable to diabetes for the IDF Diabetes Atlas: Estimates for the year 2013. Diabetes research and clinical practice 109:461-5.
-
Ma RC & Popkin BM 2017. Intergenerational diabetes and obesity—A cycle to break? : Public Library of Science San Francisco, CA USA.
-
Malseed C, Nelson A & Ware R 2014. Evaluation of a School-Based Health Education Program for Urban Indigenous Young People in Australia. Health:587-97.
-
Maple-Brown L, Lee I-L, Longmore D, Barzi F, Connors C, Boyle JA et al. 2019. Pregnancy And Neonatal Diabetes Outcomes in Remote Australia: the PANDORA study—an observational birth cohort. International journal of epidemiology 48:307-18.
-
Maple-Brown LJ & Hampton D 2020. Indigenous cultures in countries with similar colonisation histories share the challenge of intergenerational diabetes. The Lancet Global Health 8:e619-e20.
-
Minges KE, Zimmet P, Magliano DJ, Dunstan DW, Brown A & Shaw JE 2011. Diabetes prevalence and determinants in Indigenous Australian populations: a systematic review. Diabetes research and clinical practice 93:139-49.
-
NPS MedicineWise 2022. General Practice Insights Report July 2020–June 2021.
-
Rodrigues BT, Vangaveti VN & Malabu UH 2016. Prevalence and Risk Factors for Diabetic Lower Limb Amputation: A Clinic-Based Case Control Study. Journal of Diabetes Research 2016:7.
-
Sav A, King MA, Kelly F, McMillan SS, Kendall E, Whitty JA et al. 2015. Self-management of chronic conditions in a rural and remote context. Aust J Prim Health 21:90-5.
-
Shaw J & Tanamas S 2012. Diabetes: the silent pandemic and its impact on Australia. Melbourne: Baker IDI Heart and Diabetes Institute.
-
Shi B-Y 2016. The importance and strategy of diabetes prevention. Chronic diseases and translational medicine 2:204-7.
-
Thomas S 2014. The cost-effectiveness of primary care for Indigenous Australians with diabetes living in remote Northern Territory communities. The Medical Journal of Australia 201:450.
-
Titmuss A, Davis EA, Brown A & Maple‐Brown LJ 2019. Emerging diabetes and metabolic conditions among Aboriginal and Torres Strait Islander young people. Medical Journal of Australia 210:111-3. e1.
-
Voaklander B, Rowe S, Sanni O, Campbell S, Eurich D & Ospina MB 2020. Prevalence of diabetes in pregnancy among Indigenous women in Australia, Canada, New Zealand, and the USA: a systematic review and meta-analysis. The Lancet Global Health 8:e681-e98.
-
Zhao Y, Connors C, Lee AH & Liang W 2015. Relationship between primary care visits and hospital admissions in remote Indigenous patients with diabetes: A multivariate spline regression model. Diabetes Res Clin Pract 108:106-12.

