Key facts
Why is it important?
The range of harms from alcohol and other drug (AOD) use or dependence includes chronic disease (for example, liver disease and diabetes), blood-borne virus spread, injuries from motor vehicle accidents and assaults, neurological impacts, disabilities, incarceration, suicide/self-harm and social or community disruptions, including family breakdown. There is also a complex interaction between harmful AOD use and the social, historical, political and economic context of people’s lives. For some Aboriginal and Torres Strait Islander people, the legacies of colonisation, inequality and racism have led to increased vulnerability to harmful AOD use.
Mental health issues are a common comorbidity and, along with poly-drug use, means that people presenting to AOD treatment services typically have complex, multiple needs (NIDAC 2014).
Harmful AOD consumption also plays a significant role in contact with the criminal justice system and incarceration and contributes to the over-representation of Indigenous Australians in the justice and correctional systems. AOD use increases the potential for social disruption, such as domestic violence, crime and assaults (NIDAC 2014).
Indigenous Australians suffer from the harms of AOD and the burden of disease at a higher rate than non-Indigenous Australians (DoH 2017) (see measures 2.16 Risky alcohol consumption and 2.17 Drug and other substance use including inhalants). Reasons for this include disconnection to cultural values, social exclusion, discrimination and isolation, poverty, and lack of access to adequate services (DoH 2017). AOD use is a key risk factor that contributes to the health gap between Indigenous and non-Indigenous Australians (AIHW 2020; Gray et al. 2018).
Treatment services that reduce harmful AOD use can significantly reduce the level of assaults, homicides and the level of disability while improving the overall health and wellbeing of those experiencing harm from AOD (AIHW 2016). Reducing AOD related harm can improve health, social and economic outcomes at both the individual and community levels (SCRGSP 2011).
AOD treatment services provide a variety of interventions and support that seek to address harmful AOD use and restore the physical, social and emotional wellbeing of clients and their families (NIDAC 2014). Treatment services for AOD problems are composed of multiple types: withdrawal, psycho-social therapy, residential rehabilitation and pharmacotherapy maintenance. Services are delivered in a range of settings such as specialist AOD services, general health services, telephone and online interventions (Ritter et al. 2014).
Data findings
Episodes of care and treatment services
The 2017–18 Online Services Report included data from 78 Commonwealth-funded Indigenous substance-use organisations that provided 193,424 substance-use-related episodes of care to 35,331 clients (29,094 clients identified as Indigenous). The distribution of clients by remoteness categories was 41% in Major cities, 4% in Inner regional areas, 25% in Outer regional areas, 21% in Remote areas, and 10% in Very remote areas (Table D3.11.2, Table D3.11.14).
These services provided Indigenous Australians with 137,006 non-residential, follow‑up and aftercare episodes of care, such as rehabilitation and education, 22,123 sobering-up/respite episodes of care that do not include formal rehabilitation and 3,015 residential episodes of care providing temporary live-in accommodation for clients requiring formal substance-use treatment and rehabilitation (Table D3.11.2, Figure 3.11.1).
Figure 3.11.1: Episodes of care provided at Australian Government-funded Indigenous substance-use services, by type and Indigenous status, 2017–18
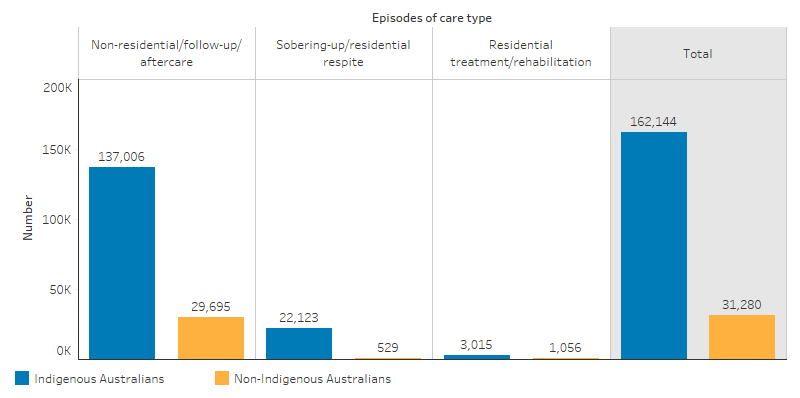
Source: Table D3.11.2. AIHW analyses of Online Services Report data collection, 2017–18.
The most common substance-use issues reported by organisations included alcohol (100%), cannabis (91%), amphetamines (80%), tobacco (62%) and multiple drug use (62%) (Table D3.11.11). Treatment types used by almost all organisations included support and case management (97%), information and education (96%) and counselling (92%) (Table D3.11.12). These organisations provided a wide range of drug and alcohol programs and activities, with the most common being community education and activities (95%), group counselling (74%), crisis intervention (71%), cultural groups (67%) and support groups (64%) (Table D3.11.13).
Social and emotional health is highly connected with issues of substance use. In 2017–18, of 78 organisations that reported on key social and emotional wellbeing related issues requiring care, 82% reported on anxiety/stress, 78% reported on depression and 78% reported on grief and loss issues as well (Table D3.11.3, Figure 3.11.2).
Figure 3.11.2: Most important social and emotional wellbeing issues reported by substance-use services in terms of staff time and organisational resources, by type of issue, 2017–18
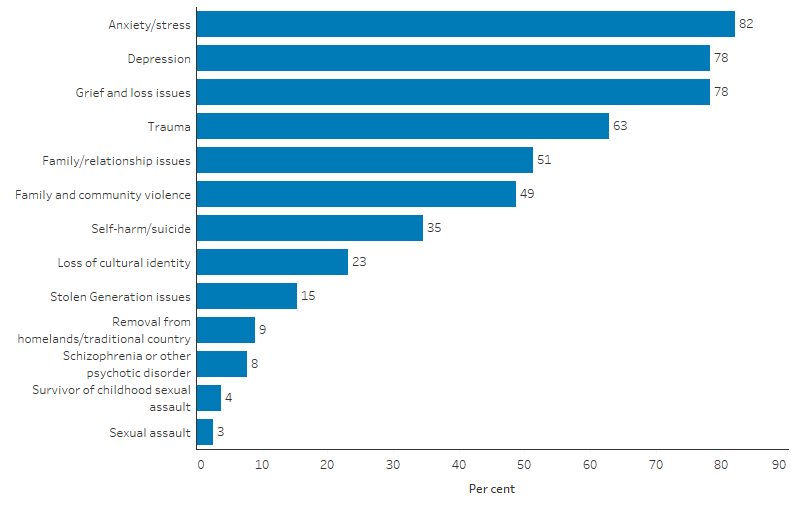
Source: Table D3.11.3. AIHW analyses of Online Services Report data collection, 2017–18.
Alcohol and other drug treatment services
The 2017–18 Alcohol and Other Drug Treatment Services National Minimum Data Set included data from 952 publicly funded alcohol and other drug (AOD) treatment agencies (some of which also reported to the Online Service Report). These services provided 32,514 closed treatment episodes to 21,387 Indigenous clients—an average of 1.5 episodes per client (Table D3.11.6). Treatment was provided to Indigenous Australians at a rate of 4,850 episodes per 100,000—5.8 times the rate for non-Indigenous Australians (838 episodes per 100,000) (Table D3.11.1).
Among Indigenous Australians, 18,988 episodes, accounting for almost 59% of all closed treatment episodes, were provided to clients aged 20–39. Among those aged 10–29, Indigenous clients had a higher proportion of closed treatment episodes compared with non-Indigenous clients (47% and 36% of episodes, respectively) (Table D3.11.1, Figure 3.11.3).
Figure 3.11.3: Closed treatment episodes for alcohol and other drug treatment, by Indigenous status and age group, 2017–18
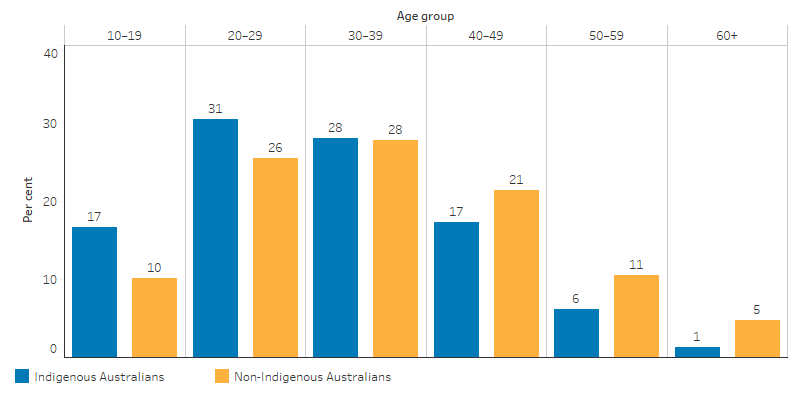
Source: Table D3.11.1. Alcohol and Other Drug Treatment Services National Minimum Data Set.
In 2017–18, Indigenous males and females were around 6 to 7 times as likely to have received a closed episode for AOD treatment (64 per 1,000 and 39 per 1,000, respectively), compared with non-Indigenous males and females (11 per 1,000 and 6 per 1,000, respectively) (Table D3.11.9).
Alcohol was the principal drug of concern for 35% of Indigenous clients (1,222 per 100,000) compared with 32% for non-Indigenous clients (166 per 100,000) and the rate at which Indigenous clients accessed treatment for alcohol use was 7 times the rate for non-Indigenous clients. For both Indigenous and non-Indigenous clients, the next highest principal drugs of concern were for cannabis (26% and 24%, respectively) and amphetamines (25% and 26%, respectively). The rate for Indigenous Australians was around 7 times the rate for non-Indigenous Australians for these drugs: 909 and 123 per 100,000, respectively, for cannabis; and 893 and 132 per 100,000, respectively, for amphetamines (Table D3.11.7, Figure 3.11.4).
Figure 3.11.4: Selected principal drugs of concern, rate of clients, by Indigenous status, 2017–18
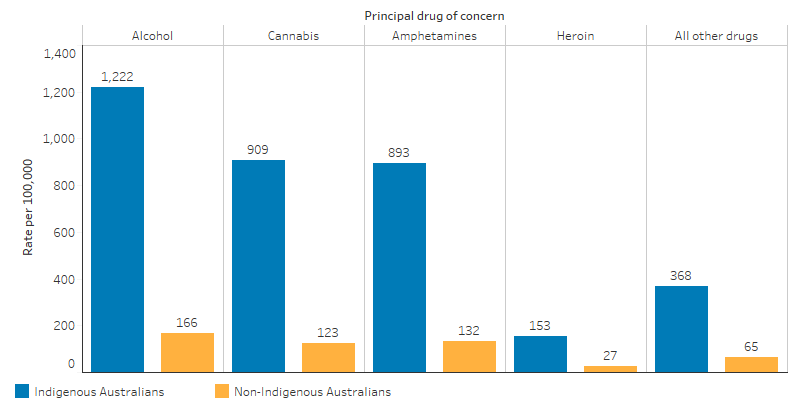
Source: Table D3.11.7. Alcohol and Other Drug Treatment Services National Minimum Data Set.
Among all Indigenous Australians aged 10 and over, the highest treatment rate for alcohol and other drugs was in the Australian Capital Territory (158 episodes per 1,000) and Victoria (133 per 1,000). The lowest rate of treatment was in Tasmania and New South Wales (19 and 33 per 1,000, respectively) (Table D3.11.9).
The main treatment types provided to Indigenous clients in 2017–18 were:
- 42% counselling
- 18% assessment only
- 11% support and case management only
- 9% information and education only (Table D3.11.8).
In 2014–15, the average distance travelled overall for treatment was greater for Indigenous clients (123 km) than for non-Indigenous clients (53 km) (AIHW 2016).
Hospitalisation from alcohol and drug use
During the period July 2015 to June 2017, there were 11,254 hospitalisations for Indigenous Australians with a principal diagnosis related to alcohol use and 12,001 hospitalisations related to drug use (Table D2.16.14, Table D2.17.8).
After adjusting for differences in the age structure between the two populations, Indigenous Australians were 3.9 times as likely to be hospitalised for alcohol use as non-Indigenous Australians (9.1 per 1,000 and 2.4 per 1,000, respectively) (Table D2.16.14, Figure 3.11.5).
Indigenous Australians were 3 times as likely to be hospitalised for a principal diagnosis related to drug use compared with non-Indigenous Australians (7.9 per 1,000 and 2.7 per 1,000) (Table D2.17.8, Figure 3.11.5).
Figure 3.11.5: Age-standardised hospitalisations with principal diagnosis related to alcohol use and drug use, by Indigenous status and sex, July 2015 to June 2017
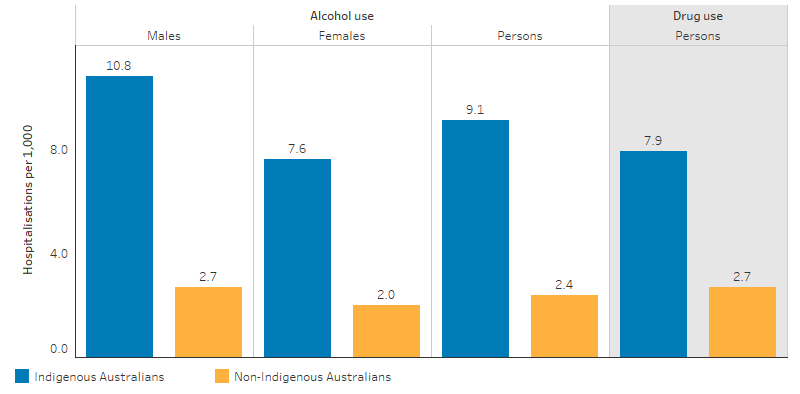
Source: Table D2.16.15, Table D2.17.8. AIHW analysis of National Hospital Morbidity Database.
General practitioner management of alcohol and drug problems
The Bettering the Evaluation and Care of Health survey (2010–15) showed that general practitioners (GPs) managed mental health–related problems for Indigenous patients in around 11% of all problems they managed. Approximately 1.4% were relating to mental health due to drug and alcohol misuse. In comparison, GPs managed mental health issues due to drug and alcohol misuse for Other Australians in fewer than 0.5% of problems they managed. After adjusting for differences in the age structure between the two populations, it showed that Indigenous Australians were significantly more likely, at 2–3 times the rate, to have these problems managed by a GP than Other Australians (12.3 and 8.6 per 1,000 compared with 3.8 and 3.9 per 1,000, respectively) (Table D1.18.21). Alcohol counselling or advice represented 1.3% of all clinical and therapeutic treatments provided to Indigenous Australians, compared with 0.7% for Other Australians (Table D3.03.6). (‘Other Australians’ includes those who were non-Indigenous and those whose Indigenous status was not stated.)
Pharmacotherapy treatment
Pharmacotherapy is one of the main treatment options for dependence on opioid drugs, such as heroin and morphine. In Australia, clients attend dosing point sites regularly to take their medication under the supervision of a pharmacist or health professional (AIHW 2018). The National Opioid Pharmacotherapy Statistics Annual Data (NOPSAD) collection provides information on a snapshot day in June 2018 on clients receiving opioid pharmacotherapy treatment. The number of Indigenous clients receiving pharmacotherapy treatment for opioid dependence at the time of the snapshot increased from 1,662 in 2006 to 3,779 in 2018, in the four jurisdictions combined with data in both periods (New South Wales, Queensland, South Australia and Australian Capital Territory) (Table D3.11.4).
In 2018, Indigenous Australians were 4.8 times as likely as non-Indigenous Australians to receive pharmacotherapy treatment (95 per 1,000 and 20 per 10,000, respectively) in the six jurisdictions with Indigenous identification data of adequate quality (New South Wales, Western Australia, South Australia, Tasmania, Australian Capital Territory and Northern Territory). Of Indigenous clients receiving pharmacotherapy treatment, 82% were aged 25–49, compared with 69% of non-Indigenous clients in this age group (Table D3.11.10). In 2018, Indigenous pharmacotherapy clients were more likely to be treated with methadone (54%) than non-Indigenous clients (41%) (AIHW 2019a).
Alcohol and drug use and treatment among prisoners
In 2018, 63% of Indigenous prison entrants had used illicit drugs and 46% reported a high risk of alcohol-related harm in the previous 12 months, compared to 66% and 26% for non-Indigenous prison entrants. Indigenous and non-Indigenous prisoners in custody had similar proportions of receiving medication for opioid dependence (1.3% and 1.5% respectively). Seven per cent of Indigenous prison dischargees reported accessing an alcohol treatment program in prison, compared with 9.5 of non-Indigenous prison dischargees (AIHW 2019b).
Research and evaluation findings
Based on results from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey (Health Survey), Indigenous Australians are about 1.4 times as likely to abstain from alcohol than non-Indigenous Australians. (This includes those who have never consumed alcohol or who have not consumed alcohol in the previous 12 months). This includes lifetime abstainers and also those who used to drink but no longer do, often as a result of the harmful effects of alcohol consumption (Wilson et al. 2010). Of the Indigenous Australians who do consume alcohol, a greater proportion drinks at levels that pose both short-term and long-term risks to their health and the health of others. After adjusting for differences in age structure, Indigenous Australians aged 15 years and over reported exceeding the alcohol guidelines for single occasion drinking at 1.2 times the rate of non-Indigenous Australians (48.5% and 41.6%, respectively). The Health Survey data also show that 28.3% of Indigenous Australians reported using substances in the previous 12 months (see measures 2.16 Risky alcohol consumption and 2.17 Drug and other substance use including inhalants).
There is evidence that the higher levels of alcohol consumption by Indigenous Australians are related to current inequalities, social disadvantage and racism, and higher levels of emotional and social distress arising from the legacy of colonialism and dispossession (Gray et al. 2018). AOD use accounts for a significant proportion of the burden of disease and injury among Indigenous Australians and alcohol use is a major contributor to unsafe communities. It is estimated that 40% of Indigenous male suicides and 30% of Indigenous female suicides were associated with alcohol (Wilson et al. 2010). AOD is also a risk factor for contact with the criminal justice system and incarceration and contributes to the over-representation of Indigenous Australians in the justice system (NIDAC 2014).
Treatment for AOD problems has been proven to have positive impacts, including reducing the consumption of AOD, improving health status, reducing criminal behaviour, improving psychological wellbeing and improving community participation (Ritter et al. 2014).
A number of factors have been identified as creating barriers to the access and provision of effective AOD treatment for Indigenous Australians (Gray et al. 2018). These include geography (for example, distance to services, transport availability and road quality); a lack of services and funding in some regions; the cultural competency of services (see measure 3.08 Cultural competency); affordability (for example, service, pharmaceutical and travel costs); and the availability of Indigenous AOD support workers, specialists and other health professionals. Additional barriers include cultural beliefs and attitudes, such as shame or community rejection associated with seeking treatment, concern about getting into trouble with the law and fear of losing access to or custody of children (NIDAC 2014).
Medication-assisted treatment for opioid dependence (MATOD) is associated with positive outcomes, including reduced risk of blood-borne virus transmission, reduced heroin-related overdoses and reduced crime associated with heroin dependence. However, it has been estimated that on any day, less than half of the Australians who are opioid-dependent are in treatment (Chalmers et al. 2009). The reasons for this include geographical difficulty in accessing treatment, being unable to access treatment during working hours and the cost. While the treatment costs are subsidised by Australian and state and territory governments, there is evidence that the dispensing and medicine administration fees by pharmacies in Australia have been a major barrier to treatment access, retention and optimal outcomes (Lord et al. 2014). Research shows that MATOD administration and dispensing fees for 12 months could be as high as $3,640 (Lord et al. 2014). These fees exist because the Pharmaceutical Benefits Scheme (PBS) does not cover daily MATOD administration and dispensing costs to pharmacies, unlike PBS items that are covered through the 7th Community Pharmacy Agreement.
Long-acting injectable buprenorphine (Buvidal and Sublocade) is the first MATOD to be covered under the PBS. This provides a treatment option of a long-lasting injection administered by a doctor or other approved health practitioner. Dispensing fees for this medicine align with standard PBS fees. While there still is an inherent cost to the service provider for administering the medicine, this may be lower per month than other existing MATOD, due to the low frequency of administration. In some cases, this cost may be borne by the service provider, such as an Aboriginal Community Controlled Health Service. This MATOD PBS subsidy has the potential to provide a significant public health benefit to reduce opioid harm by improving MATOD access for some opioid-dependent patients. There are other barriers to MATOD beyond cost, and future research on the access of this treatment by Indigenous Australians will be necessary to assess barriers further and determine how these may be overcome.
However, it is vital that the choice of MATOD is based on a clinical decision about what is the best fit for the patient and not purely based on cost. This ensures that the patient has the best chance of success. Long-acting injectable buprenorphine may not be clinically suitable for all patients.
In 2017, the Department of the Prime Minister and Cabinet commissioned the National Drug and Alcohol Research Centre to undertake a community-based participatory research project of Indigenous AOD residential rehabilitation (IAODRR) services in New South Wales. The purpose of the research project was to standardise data collection processes and models of care to inform the evidence base for AOD residential rehabilitation services in New South Wales.
The project identified the need to standardise data collection by embedding evaluation capacity into IAODRR services. Key outcomes of the project were:
- a standardised assessment tool for collecting client data on substance use, mental and physical health, quality of life and cultural connectedness
- a program logic model to define core treatment and organisational components for IAODRR services
- a standardised approach for follow-up support, including client exit interview and assessment, referral, follow up contact and assessment
- the development of an evaluation framework to evaluate costs and benefits of IAODRR services (Shakeshaft 2018).
In 2007, a 12-month trial of an evidenced-based non-residential treatment program for Indigenous clients with alcohol problems took place in Central Australia. The program offered three streams of care: pharmacotherapy, psychological and social support. An evaluation of the multi-disciplinary trial demonstrated the viability and demand for similar non-residential treatment programs (d'Abbs et al. 2013).
Implications
Due to the complex, often chronic and relapsing nature of harmful AOD use and dependence, a greater intensity of treatment services are required and these need to have a long-term focus, be broader than clinical responses and include the provision of social support services (Gray et al. 2014). Mental health issues are a common comorbidity and, along with poly-drug use, this means that people presenting to AOD treatment services typically have complex, multiple needs (NIDAC 2014).
For Indigenous Australians, these issues may be exacerbated by an increased vulnerability that has resulted from the legacies of colonisation, inequality and racism. These issues make it vitally important for the provision of culturally safe and trauma-informed treatment and healing services (Atkinson 2013). Key themes identified for effective alcohol treatment for Indigenous Australians included individual engagement, flexibility, assessment of suitability, Indigenous staff, community engagement, practical support, counselling, coping with relapse and contingency planning (Brett et al. 2014). Strategies should also address underlying social determinants, aim to prevent the uptake of harmful use, provide treatment for those who are dependent and support those whose lives are affected by others’ harmful AOD use (Gray et al. 2018).
Equity and quality of care according to the needs of Indigenous Australians are important considerations in health service planning. Large Indigenous Australian populations in some regions are under-serviced, and there is limited coverage of Indigenous-specific AOD detoxification, treatment, support, intervention and aftercare services. There is a lack of Indigenous-specific AOD treatment and support services targeting women, families, young people and patients with co-morbid mental health issues (Gray & Wilkes 2010). Other specific gaps in the provision of AOD services include those providing ongoing care (including care following intensive treatment) and treatment services in correctional institutions.
More research needs to be undertaken on the barriers for Indigenous Australians in terms of accessing AOD treatment and support services and determining the level of met or unmet need. Additional research would also help in understanding how cultural beliefs and attitudes can be a barrier to accessing services.
The policy context is at Policies and strategies.
References
- AIHW (Australian Institute of Health and Welfare) 2016. Alcohol and other drug treatment services in Australia 2014–15. Drug treatment series no. 27. Cat. no. HSE 173. Canberra: AIHW.
- AIHW 2018. National opioid pharmacotherapy statistics (NOPSAD) 2017. Canberra: AIHW.
- AIHW 2019a. National Opioid Pharmacotherapy Statistics Annual Data collection (NOPSAD) 2018 web report. Cat. no. HSE 218. Canberra: AIHW.
- AIHW 2019b. The health of Australia’s prisoners 2018. Cat. no. PHE 246. Canberra: AIHW.
- AIHW 2020. Alcohol, tobacco & other drugs in Australia. Canberra: AIHW.
- Atkinson J 2013. Trauma-informed services and trauma-specific care for Indigenous Australian children. Closing the Gap Clearinghouse. Canberra: Australian Institute of Health and Welfare & Australian Institute of Family Studies.
- Brett J, Lawrence L, Ivers R & Conigrave K 2014. Outpatient alcohol withdrawal management for Aboriginal and Torres Strait Islander Australians. Australian Family Physician 43:563-6.
- Chalmers J, Ritter A, Heffernan M & McDonnell G 2009. Modelling pharmacotherapy maintenance in Australia: exploring affordability, availability, accessibility and quality using system dynamics. ANCD Research Paper 19.
- d'Abbs P, Togni S, Rosewarne C & Boffa J 2013. The Grog Mob: lessons from an evaluation of a multi‐disciplinary alcohol intervention for Aboriginal clients. Australian and New Zealand journal of public health 37:450-6.
- DoH (Australian Government Department of Health) 2017. National drug strategy 2017–2026. Commonwealth of Australia Canberra.
- Gray D, Cartwright K, Stearne A, Saggers S, Wilkes E & Wilson M 2018. Review of the harmful use of alcohol among Aboriginal and Torres Strait Islander people. Australian Indigenous HealthInfoNet.
- Gray D, Stearne A, Bonson M, Wilkes E, Butt J & Wilson M 2014. Review of the Aboriginal and Torres Strait Islander Alcohol, Tobacco and Other Drugs Treatment Service Sector: Harnessing Good Intentions (Revised Version). Perth, WA: NDRI.
- Gray D & Wilkes E 2010. Reducing alcohol and other drug related harm. Closing the Gap Clearinghouse. Canberra: Australian Institute of Health and Welfare & Australian Institute of Family Studies.
- Lord S, Kelsall J, Kirwan A & King T 2014. Opioid pharmacotherapy fees: A long-standing barrier to treatment entry and retention. Policy Brief.
- NIDAC (National Indigenous Drug and Alcohol Committee) 2014. Alcohol and other drug treatment for Aboriginal and Torres Strait Islander peoples. Canberra: ANCD.
- Ritter A, Berends L, Chalmers J, Hull P, Lancaster K & Gomez M 2014. New Horizons: The review of alcohol and other drug treatment services in Australia. Drug Policy Modelling Program, National Drug and Alcohol Research Centre.
- SCRGSP (Steering Committee for the Review of Government Service Provision). 2011. Overcoming Indigenous disadvantage: Key indicators 2011. Canberra, Productivity Commission.
- Shakeshaft A, Clifford A, James D, Doran C, Munro A, Patrao T, Bennett A, Binge C, Bloxsome T, Coyte J, Edwards D, Henderson N, Jeffries D. 2018. Understanding clients, treatment models, and evaluation options for the NSW Aboriginal Residential Healing Drug and Alcohol Network (NARHDAN): a community-based participatory research approach. National Drug and Alcohol Research Centre (UNSW Sydney).
- Wilson M, Stearne A, Gray D & Saggers S 2010. The harmful use of alcohol amongst Indigenous Australians. Australian Indigenous HealthInfoNet.

