Key messages
- In 2015–2019, 5.5% of deaths among Indigenous Australians were due to suicide (847 deaths), and 3.7% were due to mental health-related conditions (574 deaths) (such as injury or non-psychiatric illness affecting the brain).
- Over the decade 2010 to 2019, the age-standardised rate of suicide for Indigenous Australians increased from 20 to 27 per 100,000 population (30% increase), while the rate for non-Indigenous Australians increased from 11 to 13 per 100,000 population (24% increase).
- From 2009–10 to 2018–19, the hospitalisation rate for mental health-related conditions increased from 18 to 29 per 1,000 population for Indigenous females and from 20 to 30 per 1,000 for Indigenous males. The hospitalisation rate for intentional self-harm increased from 2.6 to 4.4 per 1,000 population for Indigenous females and from 2.0 to 2.7 per 1,000 population for Indigenous males.
- In 2018–19, National Aboriginal and Torres Strait Islander Health Survey participants who were removed, or whose relatives were removed from their family, were more likely to have high levels of psychological distress (38%) than those who had not been removed nor had a family member removed (26%).
- Employment status and housing tenure have been associated with health and wellbeing outcomes. Multivariate analysis of the ABS health and social surveys has shown that Indigenous Australians who were employed had better health and wellbeing outcomes than those who were unemployed. Additionally, Indigenous Australians who were renting had lower health and wellbeing outcomes compared with Indigenous property owners.
- A review of research focused on Indigenous peoples from Canada, Australia, New Zealand and the United States found that culture is significantly and positively associated with physical health, social and emotional wellbeing, and reduces risk-taking behaviours.
- Suicide prevention studies have identified the need to focus on protective factors, such as community connectedness, strengthening the individual and rebuilding family, as well as culturally based programs.
Why is it important?
Social and emotional wellbeing is the foundation for physical and mental health for Aboriginal and Torres Strait Islander people (Commonwealth of Australia 2017). It is holistic, in that it results from a network of relationships between individuals, family, kin and community. Indigenous Australians’ experience of social and emotional wellbeing varies across different cultural groups as well as across individuals. The concept of social and emotional wellbeing also recognises that a person’s wellbeing is influenced by the social determinants of health, engendered through the inequity of government policies, institutional racism, the effects of colonisation and other past events. For Indigenous Australians, health is not just the physical wellbeing of the individual but the ‘social, emotional and cultural wellbeing of the whole community’, and is based on connections to country, culture, community, family, spirit and physical and mental health (Dudgeon et al. 2014; Gee et al. 2014; Parker & Milroy 2014; Social Health Reference Group 2004). The National Strategic Framework for Aboriginal and Torres Strait Islander Peoples’ Mental Health and Social and Emotional Wellbeing 2017–2023 proposes a model of social and emotional wellbeing with seven overlapping domains comprising: body; mind and emotions; family and kin; community; culture; country; and spirituality and ancestors (Commonwealth of Australia 2017; Gee et al. 2014).
Culture and cultural identity are critical foundations of a person’s social and emotional wellbeing and their capacity to lead successful and fulfilling lives. The social determinants of health are the conditions in which people are born, grow, live, work and age, and are mostly responsible for health inequalities (WHO 2020). The causes of inequality have been identified as unequal access to health care, schools and education, conditions of work and leisure, housing, and the associated chances of leading a healthy life (Australian Psychological Society 2018). The antecedents of which are due to the structural disadvantage brought about by social policy, economic systems and the distribution of power and resources.
Social determinants of health have a strong impact on social and emotional wellbeing. The social determinants of health, including education, employment, income and position within Australian society, have been linked with other external stressors such as serious illness, disability, inadequate housing, inaccessibility of reliable utilities, overcrowding, exposure to violence including family violence, substance misuse, incarceration, and interpersonal and institutional racism. Taken together, many of the negative effects upon the social and emotional wellbeing of Indigenous Australians arises from their ongoing experience of entrenched disadvantage.
This experience of disadvantage is further reflected in Indigenous Australians’ experience in mainstream health care. It has been shown that traditional western models of health treatment, including failure to communicate effectively, can result in discharge against medical advice by Indigenous patients, which could be avoided with improvements to institutional cultural safety (Einsiedel et al. 2013). Peak Indigenous health bodies argue that culturally safe and culturally competent clinical care may substantially contribute to Indigenous health improvement (Laverty et al. 2017). It follows that a more specific embedding of cultural safety within mandatory standards for safe, quality-assured and culturally competent clinical care may strengthen the health system in delivering care that meets the needs of Indigenous Australians (see measure 3.08 Cultural competency).
Social and emotional wellbeing problems are distinct from mental health problems and mental illness, although they can interact and influence each other (Commonwealth of Australia 2017). The National Strategic Framework for Aboriginal and Torres Strait Islander Peoples’ Mental Health and Social and Emotional Wellbeing 2017–2023 recognises this distinction. Even with good social and emotional wellbeing, people can experience mental illness. People with mental health problems or mental illness can live and function at a high level with adequate support, and continue to have social and emotional wellbeing needs. Mental health is a positive state of wellbeing in which a person can manage their thoughts and feelings to cope with the normal stress of life and reach their potential in work and community life in the context of family, community, culture and broader society. Mental health problems are ‘diminished cognitive, emotional or social abilities but not to the extent that the criteria for a mental illness are met’, for example psychological distress. Mental illnesses are diagnosed according to certain criteria. They range from high prevalence disorders such as anxiety and depression, through to low prevalence disorders such as psychosis, schizophrenia, and bi-polar disorder.
The COVID-19 pandemic has posed, and continues to pose, a high risk to Indigenous Australians’ physical and social and emotional wellbeing (Victorian Government et al. 2020). Specific concerns have included: lack of accessible, culturally appropriate and culturally safe mental health services; challenges faced by the Indigenous Australian allied health workforce, including those living with high-risk individuals; inequalities within the health system that may affect access to care, particularly in the move to digital and telehealth; and loss of remote community services including fly in fly out mental health care. As a population group, Indigenous Australians were identified as being at greater risks of COVID-19, due to factors such as higher rates chronic health conditions and multimorbidity, socioeconomic inequities, and poorer access to services (Crooks et al. 2020; Department of Health 2020; Yashadhana et al. 2020). For example, overcrowded housing (experienced at higher rates among the Indigenous population) can make safe isolation infeasible, and lower levels of income can impact the ability to purchase personal protective equipment (e.g. masks).
Moreover, the impact of lockdowns is particularly acute for Indigenous Australians who are deeply interconnected with family and community members, and where caring responsibilities may have been disrupted. There are heightened effects on those in, or with connections to, remote communities, where isolation has been greater and freedom of movement more restricted; those who cannot access waterways, songlines and country; and those who cannot attend to cultural and sorry business (Victorian Government et al. 2020). Research on the impacts of COVID-19 and the associated restrictions on Stolen Generations survivors found they had an increased and heightened sense of isolation and loneliness, significant disconnection from family, community, culture and country, and declines in their mental health and wellbeing (Aboriginal and Torres Strait Islander Healing Foundation 2021). Tailored, collaboratively built solutions are needed, with Indigenous Australians taking leadership of and being engaged in shared decision-making regarding mental health supports to ensure they are culturally competent, safe and sustainable.
In July 2020, the National Agreement on Closing the Gap (the National Agreement) identified the importance of enjoying high levels of social and emotional wellbeing. The National Agreement has recognised the importance of Indigenous Australians enjoying high levels of social and emotional wellbeing by establishing the following outcome and target to direct policy attention and monitor progress:
- Target 14 — Significant and sustained reduction in suicide of Aboriginal and Torres Strait Islander people towards zero.
The National Agreement has also recognised that strong Aboriginal and Torres Strait Islander cultures are fundamental to improved life outcomes for Indigenous Australians and that all activities to be implemented under the Agreement need to support, promote and not diminish these cultures. In particular, the Agreement has established the following targets to support the cultural wellbeing of Indigenous Australians:
- Target 15a — By 2030, a 15 per cent increase in Australia’s landmass subject to Aboriginal and Torres Strait Islander people’s legal rights or interests.
- Target 15b — By 2030, a 15 per cent increase in areas covered by Aboriginal and Torres Strait Islander people’s legal rights or interests in the sea.
- Target 16 — By 2031, there is a sustained increase in number and strength of Aboriginal and Torres Strait Islander languages being spoken.
For the latest data on the Closing the Gap targets, see the Closing the Gap Information Repository.
The National Aboriginal and Torres Strait Islander Health Plan 2021-2031 (the Health Plan), released in December 2021, provides a strong overarching policy framework for Aboriginal and Torres Strait Islander health and wellbeing. The Health Plan was developed in genuine partnership with Aboriginal and Torres Strait Islander leaders and is the first national health document to address the health targets and priority reforms of the National Agreement.
Priority 6 of the Health Plan focuses on ‘Social and emotional wellbeing and trauma-aware, healing-informed approaches’ to service delivery, and includes the following objectives:
- Objective 6.1 Update and implement a strategic approach for social and emotional wellbeing
- Objective 6.2 Support Aboriginal Community Controlled Health Services to deliver social and emotional wellbeing services
- Objective 6.3 Support Aboriginal and Torres Strait Islander organisations to provide leadership on healing and social and emotional wellbeing
- Objective 6.4 Implement training and other support across the whole health system to better understand and respond to social and emotional wellbeing in all aspects of life.
Priority 10 of the Health Plan focuses on mental health and suicide prevention. A number of objectives focus on strengthening culturally safe suicide prevention services, improving continuity of care, and implementing key reforms to Indigenous mental health and suicide prevention policy.
See the Intentional self-harm deaths (suicide) section in this measure for data on suicide. Non-fatal hospitalisations for intentional self-harm and hospitalisations for mental health-related disorders have been identified as supporting indicators for the target, and information on these is also contained in this measure.
Burden of disease
In 2018, mental and substance use disorders were estimated to cause 54,263 years of healthy life lost (disability-adjusted life years or DALY). The mental and substance use disorders disease group was the leading cause (23%) of total disease burden for Indigenous Australians, and was responsible for 42% of the non-fatal burden (YLD) (46% for males and 38% for females).
The conditions contributing the most burden in this disease group were:
- anxiety disorders (23% of burden due to mental and substance use disorders)
- alcohol use disorders (19%)
- depressive disorders (19%)
- drug use disorders (9%)
- schizophrenia (7%).
After adjusting for differences in the age-structure between the two populations, the rate of total burden due to mental and substance use disorders for Indigenous Australians was 2.8 times the rate for non-Indigenous Australians (70 and 25 DALY per 1,000 people, respectively). Mental and substance use disorders were the top contributor to the gap in disease burden between Indigenous and non-Indigenous Australians, accounting for one-fifth (20%) of the total gap (AIHW 2022c).
Data findings
Findings from ABS survey data
The 2018–19 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS) collected information on a range of topics relevant to social and emotional wellbeing. The survey showed that Indigenous Australians retain links to their culture and family connections. In 2018–19, 66% (314,170) of Indigenous Australians aged 15 and over identified with a tribal/language group or clan and 74% (357,420) recognised an area as homelands/traditional country (Table D1.18.1).
In 2018–19, of NATSIHS survey participants who were able to state whether they or a family member had been removed, 54% (214,200) reported that they and/or a relative had been removed from their natural family. Those who were removed or whose relatives were removed from their family were more likely to have high levels of psychological distress (38%; 81,165) than those who had not been removed nor had a family member removed from their family (26%; 133,105) (Table D1.18.5).
The 2014–15 National Aboriginal and Torres Strait Islander Social Survey (NATSISS) provides broad, reported information across key areas of social interest for Aboriginal and Torres Strait Islander people. In 2014–15, 63% (277,700) of Indigenous Australians aged 15 and over were involved in cultural events, ceremonies or organisations in the last 12 months, 92% (406,400) could get support in a time of crisis and 97% (429,800) reported that they had been involved in sporting, social or community activities in the last 12 months (Table D1.13.3, Table D1.13.4).
The NATSISS included an overall life satisfaction measure with a scale from 0 ‘not at all satisfied’ to 10 ‘completely satisfied’ (ABS 2016). More than half (53%; 236,700) of Indigenous Australians aged 15 and over reported an overall life satisfaction rating of 8 or above (52% in non-remote areas and 58% in remote areas). A high rating of 10 was more common in remote areas (Remote and Very remote areas combined) (27%; 26,200), than non-remote areas (Major cities, Inner and Outer regional areas combined) (14%; 49,100).
More than half (53%; 236,700) of Indigenous Australians aged 15 and over reported an overall life satisfaction rating of 8 or above (52% in non-remote areas and 58% in remote areas). A high rating of 10 was more common in remote areas (27%; 26,200) than non-remote areas (14%; 49,100).
The life satisfaction rating of 8 or above for Indigenous Australians was associated with: a self-assessed health status of excellent or very good (67% compared with 37% of those with fair/poor health); being employed (61% compared with 41% for those who were unemployed); and not experiencing violence in the last 12 months (57% compared with 39% of those who did experience violence) (Figure 1.18.1) (ABS 2016).
Figure 1.18.1: Proportion of Indigenous Australians aged 15 and over reporting high life satisfaction ratings, by selected characteristics 2014–15
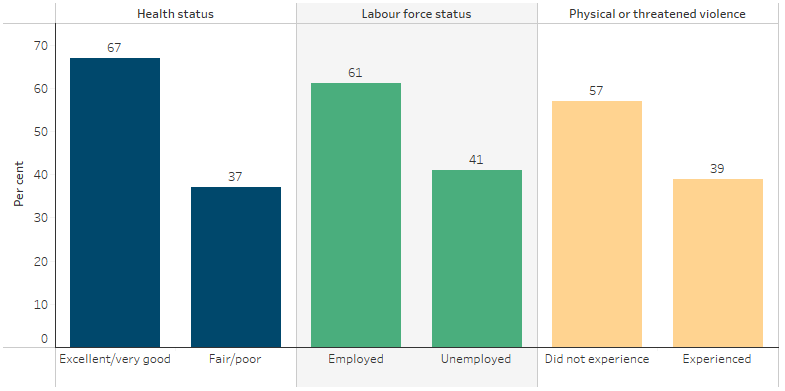
Source: AIHW and ABS analysis of the National Aboriginal and Torres Strait Islander Social Survey 2014–15 (ABS Table 17.3).
Based on analysis of the 2008 NATSISS and the Household Income and Labour Dynamics in Australia Survey (HILDA), 53% of Indigenous Australians reported that they had ‘been a happy person’ all or most of the time in the previous four weeks, compared with 61% of non-Indigenous Australians (AIHW 2014). Higher levels of education and being employed were associated with higher levels of wellbeing (Kahneman & Deaton 2010). However, there was a weaker link between income and positive wellbeing for Indigenous Australians in remote areas compared with non-remote areas.
Further analysis of HILDA results over the period 2001–12 showed that life satisfaction ratings peaked in 2003 for both Indigenous and non-Indigenous Australians, but declined significantly after that point for Indigenous Australians only (Manning et al. 2016).
Psychological distress
The 2018–19 National Aboriginal and Torres Strait Islander Survey showed that 67% of Indigenous Australians aged 18 and over had low/moderate levels of psychological distress and 31% had high/very high levels, up 4 percentage points since 2004–05 (27%). The proportion of non-Indigenous Australians reporting high/very high levels of psychological distress was 13% in both 2004–05 and 2018–19 (Table D1.18.35, Figure 1.18.2).
Figure 1.18.2: Proportion of people aged 18 years and over reporting high/very high levels of psychological distress (age-standardised), by Indigenous status, 2004–05, 2008, 2012–13, 2014–15 and 2018–19
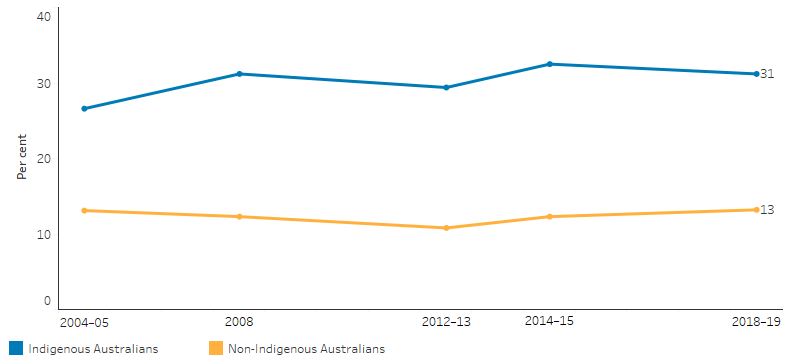
Source: Table D1.18.35. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2004–05, 2008, 2014–15, 2018–19; National Health Survey, 2004–05, 2007–08, 2014–15, 2017–18; Australian Aboriginal and Torres Strait Islander Health Survey 2012–13 (2012–13 NATSIHS component); Australian Health Survey 2012–13.
In 2018–19, after adjusting for differences in the age structure between the two populations, Indigenous adults were 2.4 times as likely as non-Indigenous adults to experience high levels of psychological distress (31% compared with 13%).
Indigenous females were more likely than Indigenous males to report high levels of psychological distress (35% compared with 26%). By remoteness, the proportion of Indigenous adults reporting high levels of psychological distress was 32% in non-remote areas and 28% in remote areas (Table D1.18.3).
In 2018–19, Indigenous adults reporting high levels of psychological distress were more likely to:
- have lower income (44% compared with 18% of those with high income),
- be unemployed (42% compared with 22% for those who were employed),
- smoke (38% compared with 27% for non-smokers),
- have a disability (46% compared with 18% for those with no disability), and
- have three or more long-term health conditions (42% compared with 15% for those with no long-term health conditions) (Table D1.18.6, Table D1.18.7, Figure 1.18.3).
Figure 1.18.3: Proportion of Indigenous Australians aged 18 and over reporting high/very high levels of psychological distress, by selected socioeconomic and health factors, 2018–19
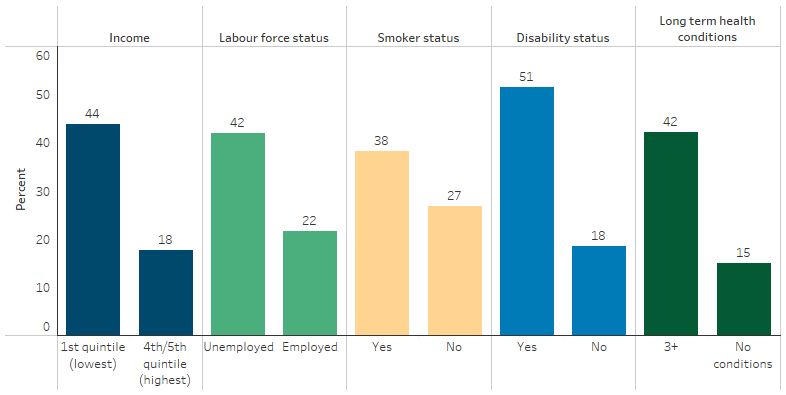
Source: Table D1.18.6 and D1.18.7. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
Life stressors
The 2014–15 NATSISS showed that 68% of Indigenous Australians aged 15 and over had experienced one or more stressors in the last 12 months. The most reported stressors for Indigenous Australians were death of a family member or close friend (28%), inability to get a job (19%), serious illness (12%) and mental illness (10%). Indigenous Australians experienced an average of two stressors in the last 12 months (Table D1.18.4, Figure 1.18.4).
Figure 1.18.4: Personal stressors experienced in the last 12 months, Indigenous Australians aged 15 and over, 2014–15
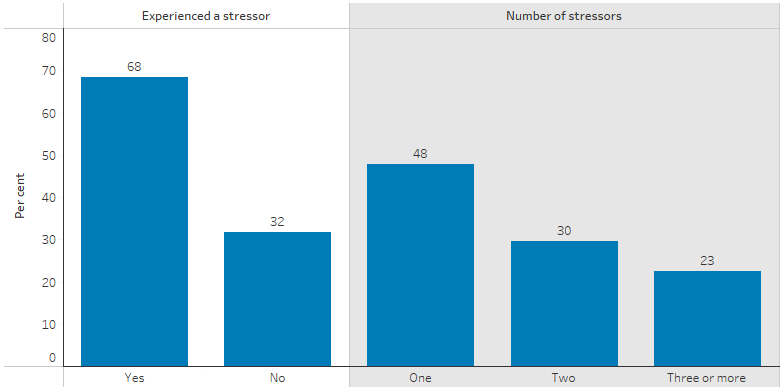
Source: Table D1.18.4. AIHW and ABS analysis of the National Aboriginal and Torres Strait Islander Social Survey 2014–15.
Compared with Indigenous Australians living in remote areas, those in non-remote areas were more likely to report stressors due to serious illness (13% compared with 9%), mental illness (12% compared with 6%) and discrimination (5.0% compared with 3.6%). Compared with Indigenous Australians living in non-remote areas, those living in remote areas were more likely to report stressors such as the death of a family member or close friend (35% compared with 26%), overcrowding (9.3% compared with 5.8%) or alcohol problems (8.9% compared with 5.9%) (Table D1.18.4).
Depression and racism
The 2018–19 National Aboriginal and Torres Strait Islander Health Survey showed that 25% (109,350) of Indigenous Australians aged 15 and over felt that they had been treated unfairly in the last 12 months because they were Aboriginal and/or Torres Strait Islander. Rates of high/very high psychological distress were higher for this group (45%; 48,795) than for those who reported that they had not been treated unfairly (28%; 91,890) (Table D1.18.5).
Social and emotional wellbeing of children
The 2014–15 National Aboriginal and Torres Strait Islander Social Survey showed that 67% (116,500) of Indigenous children aged 4–14 were reported to have experienced one or more stressors in the last 12 months. The most commonly reported stressors were death of family/friend (25%; 43,500), being scared or upset by an argument or someone’s behaviour (23%; 40,000) and trouble keeping up with school work (23%; 39,800). In addition, 40% (68,900) of Indigenous children aged 4–14 had been bullied at school and 9% (15,300) had been treated unfairly at school because they were Aboriginal and/or Torres Strait Islander (ABS 2016).
A similar proportion of Indigenous Australians aged 15 and over reported to have experienced stressors in the last year, with death of family or friend (28%; 122,384) and unable to get a job (19%; 82,033) being the most common concerns. Some concerns were higher for Indigenous Australians living in remote areas than others in non-remote areas. For example, 35% of Indigenous Australians in remote areas reported stress over the death of family or friend, compared with 26% for those living in non-remote areas. Overcrowding at home (9.3%; 9,000) and alcohol-related problems (8.9%; 8,600) were also more common for people living in remote areas.
Mental health conditions
In the 2018–19 National Aboriginal and Torres Strait Islander Health Survey, 24% (187,500) of Indigenous Australians aged 18 years and over reported having a current, diagnosed long-term mental health condition (ABS 2019). The most commonly reported long-term mental health conditions for Indigenous adults were depression or feeling depressed (78%), anxiety or feeling anxious or nervous (78%), behavioural or emotional problems (30%) and harmful use of drugs or alcohol (14%) (Table D1.18.33). Indigenous males aged 18 and over were less likely to report having a mental health condition than Indigenous females (25% compared with 34%) (Table D1.18.33). Indigenous young people aged 0–14 (15%) were less likely to report having a mental health condition than those aged 25 and over (ranging from 27% to 32%) (ABS 2019).
Two in five (39%) Indigenous Australians reported having ever been diagnosed with a mental health condition, this proportion was lower for Indigenous males (33%) than for Indigenous females (44%). Those in remote areas were less likely than those in non-remote areas to report having ever been diagnosed with a mental health condition. Of those who reported any mental health condition diagnosis, the most commonly reported conditions were depression or feeling depressed (76%), anxiety or feeling anxious (68%) and harmful use or dependence on alcohol or drugs (24%). These outcomes were relatively consistent across sex and area of remoteness (Table D1.18.43).
The 2014–15 NATSISS found that Indigenous Australians aged 15 and over with a mental health condition were more likely than those with no long-term health conditions to:
- be a daily smoker (46% compared with 39%),
- have used harmful substances in the last 12 months (39% compared with 29%),
- report experiencing one or more personal stressors in the last 12 months (84% compared with 60%),
- have experienced physical violence in the last 12 months (20% compared with 12%),
- have experienced problems accessing health services (23% compared with 10%) (ABS 2016).
Indigenous Australians aged 15 and over with a mental health condition were less likely to have had daily face-to-face contact with family or friends outside their household (36%) than those with no long-term health conditions (52%) (ABS 2016).
Mental health-related deaths (not including intentional self-harm)
Over the period 2015–2019, mental health-related conditions accounted for 3.7% (or 574) of all deaths for Indigenous Australians in the five jurisdictions for which the Indigenous identification in deaths data is considered to be of adequate quality (New South Wales, Queensland, Western Australia, South Australia and the Northern Territory) (Table D1.18.13, Table D1.23.1).
Of these deaths, 65% (374) were from organic and symptomatic mental disorders (injury or non-psychiatric illness affecting the brain) and 20% (112) were from mental and behavioural disorders due to psychoactive substance use (Table D1.18.13).
Indigenous females had a slightly higher death rate due to mental health-related conditions compared with Indigenous males (60 and 54 per 100,000, respectively) (Table D1.18.12).
For Indigenous and non-Indigenous Australians, the death rate for mental health-related conditions increased with age and was highest for those aged 75 and over. Death rates were similar between Indigenous males and females across most age groups, the exception being those aged between 45 and 64. The relative difference was greatest for those aged 45–54, where the rate for Indigenous males was 3.4 times that of Indigenous females (18 and 5.2 per 100,000, respectively) (Table D1.18.12).
After adjusting for differences in the age structure between the two populations, Indigenous Australians died from mental health-related conditions at a slightly higher rate than non-Indigenous Australians (rate ratio 1.2).
Intentional self-harm deaths (suicide)
In the combined years 2015–2019, in total across New South Wales, Queensland, Western Australia, South Australia and the Northern Territory:
- There were 847 Indigenous deaths from intentional self-harm (suicide), a rate of 24 suicide deaths per 100,000 population.
- Suicide accounted for approximately 5.5% of Indigenous deaths (Table D1.18.30, Table D1.23.1).
- Indigenous males accounted for nearly three quarters (73%) of suicide deaths in the Indigenous population (similar to the proportion for non-Indigenous males of 76%).
- The suicide rate for Indigenous Australians was highest for those in Western Australia (36 per 100,000), followed by the Northern Territory (29 per 100,000), Queensland (26 per 100,000), South Australia (18 per 100,00) and New South Wales (17 per 100,000).
- For Indigenous Australians in Western Australia the suicide rate was 2.2 times the rate for Indigenous Australians in New South Wales (Table D1.18.30).
After adjusting for differences in the age structure between the two populations, the suicide rate for Indigenous Australians was twice as high as the rate for non-Indigenous Australians.
During 2015–2019, the majority (85%; 719) of suicides by Indigenous Australians occurred in those aged under 45. This pattern was different among non-Indigenous Australians, where 49% of deaths by suicide occurred in those aged under 45 years (Table D1.18.22, Figure 1.18.5).
Figure 1.18.5: Death rates due to suicide, by Indigenous status, sex and age group, NSW, Qld, WA, SA and the NT, 2015–2019
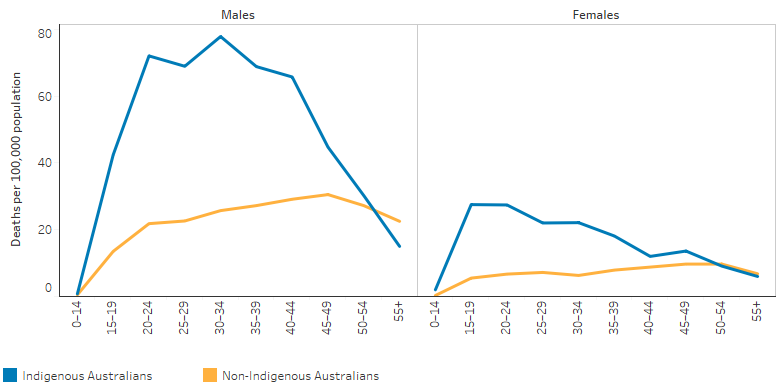
Source: Table D1.18.22. AIHW National Mortality Database.
Mental health conditions managed by a general practitioner
In 2010–15, around 11% of all problems managed by general practitioners (GP) for Indigenous patients were mental health-related. Depression was the leading mental health problem managed by GPs for Indigenous and Other Australians (both 2.9% of all problems). Other Australians includes non‑Indigenous Australians and those whose Indigenous status is unknown.
After adjusting for differences in the age structure between the two populations, GPs managed mental health-related problems for Indigenous Australians at 1.2 times the rate for Other Australians (Table D1.18.21).
Hospitalisation for mental health-related conditions (excluding intentional self-harm)
Between July 2017 and June 2019, there were 47,096 hospitalisations with a principal diagnosis of mental health-related conditions for Indigenous Australians – 7.7% of all hospitalisations excluding dialysis (or 4.3% of total hospitalisations).
Indigenous males were hospitalised for mental health-related conditions at twice the rate of non-Indigenous males, and Indigenous females at 1.6 times the rate for non-Indigenous females (Table D1.18.15, Table D1.02.3).
The most common mental health-related conditions leading to hospitalisation for Indigenous Australians were psychoactive substance use (38% of hospitalisations for mental health-related conditions; 17,818 hospitalisations), schizophrenia (22%; 10,271), neurotic, stress-related disorders (14%; 6,411) and mood disorders (13%; 6,269) (Table D1.18.17).
The hospitalisation rates for Indigenous Australians for mental-health-related conditions was lowest in Inner regional areas (22 hospitalisations per 1,000 population) and highest in Remote areas (33 per 1,000) (Table D1.18.16). Rates also varied by jurisdiction; they were lowest in Tasmania (17 per 1,000) and highest in South Australia (36 per 1,000) (Table D1.18.38).
By age group, hospitalisation rates for Indigenous Australians for mental health-related conditions were highest for those aged 35–44 (Table D1.18.14, Figure 1.18.6). The hospitalisation rate was higher for Indigenous Australians than non-Indigenous Australians in all 10-year age groups between 5–14 and 55–64. After adjusting for differences in the age structure between the two populations, Indigenous Australians were hospitalised for mental health-related conditions at 1.8 times the rate for non-Indigenous Australians (Table D1.18.15)
Figure 1.18.6: Age-specific hospitalisation rates for a principal diagnosis of mental health-related conditions, by Indigenous status and age group, Australia, July 2017 to June 2019
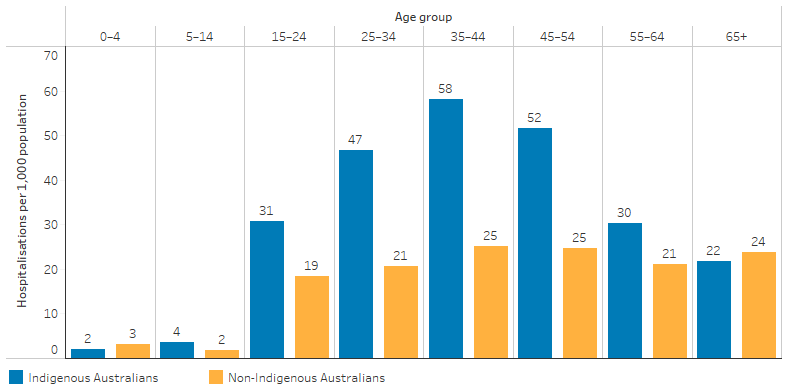
Source: Table D1.18.14 AIHW analysis of National Hospital Morbidity Database.
Hospitalisation for intentional self-harm
Between July 2017 and June 2019, there were 5,829 hospitalisations of Indigenous Australians due to intentional self-harm (0.9% of all hospitalisations of Indigenous Australians, excluding dialysis) (Table D1.18.28, Table D1.02.3). Hospitalisation rates for intentional self-harm were higher for Indigenous females (4.4 hospitalisations per 1,000 population) than for Indigenous males (2.6 per 1,000). Hospitalisations from injury and poisoning and a first reported external cause of self-harm were highest for Indigenous males aged 35–44 (5.2 per 1,000) and Indigenous females aged 15–24 (9.2 per 1,000) (Table D1.18.27).
Rates of hospitalisation for intentional self-harm for Indigenous Australians varied between jurisdictions, with the lowest rates in Tasmania (2.0 per 1,000) and the highest in Australian Capital Territory (4.8 per 1,000). After adjusting for differences in the age structure between the two populations, Indigenous Australians were hospitalised for intentional self-harm at 3 times the rate for non‑Indigenous Australians (Table D1.18.28).
Social and emotional wellbeing workforce
Statistical Areas Level 2 (SA2s) are part of the Australian Statistical Geography Standard main structure, with populations generally ranging from 3,000 to 25,000 people, and are designed to reflect communities that interact socially and economically. In 2017, the number of employed psychologists was lowest in SA2s that had a high proportion of Indigenous Australians in the population.
In 2017, there were 37 full-time equivalent employed psychologists per 100,000 population in SA2s with 20% or more Indigenous Australians in the population, compared with 131 per 100,000 in SA2s with less than 1% of Indigenous Australians in the population (Table D3.22.17) (see measure 3.22 Recruitment and retention of staff).
In 2017–18, 55% (108) of the 198 Australian Government funded Indigenous primary health-care organisations provided mental health promotion activities (Table D3.03.9). As at 30 June 2018, these organisations employed 534 full-time equivalent (FTE) social and emotional wellbeing staff and 57% of these staff were Indigenous (Table D3.12.15). A further 42 FTE social and emotional wellbeing positions were vacant, with a 7.3% vacancy rate (Table D3.22.11). These staff provided over 217,100 client contacts for social and emotional wellbeing in 2017–18, the majority of which were for Indigenous clients (86% or 186,500) (AIHW 2019a). The main service gap reported by Indigenous primary health-care organisations was mental health/social and emotional health and wellbeing, with 68% of organisations reporting this as one of their top five service gaps (Table D3.14.56).
For more information, see measures 3.03 Health promotion, 3.10 Access to mental health services, and 3.14 Access to services compared to need.
Change over time (deaths and hospitalisation)
Between 2006 and 2019, the age-standardised suicide rate for Indigenous Australians increased from 18 to 27 per 100,000 population (58%). Over this period, the suicide rate for non-Indigenous Australians also increased, though to a lesser extent, from 10 to 13 per 100,000 population (33% increase). These data are for New South Wales, Queensland, Western Australia, South Australia and the Northern Territory combined.
Over the decade 2010 to 2019, the suicide rate for Indigenous Australians increased by 30% (from 20 to 27 per 100,000 population), while the rate for non-Indigenous Australians increased by 24% (from 11 to 13 per 100,000 population), based on age-standardised rates. The gap in the suicide rates for the two populations widened by 38% over the period (Table D1.18.24, Figure 1.18.7).
Figure 1.18.7: Age-standardised death rates and changes in the gap due to suicide, by Indigenous status, NSW, Qld, WA, SA and NT, 2006 to 2019
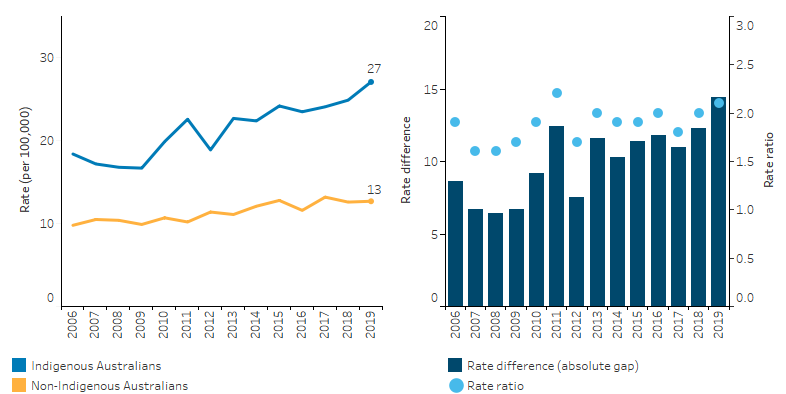
Note: Rate difference is the age-standardised rate (per 100,000) for Indigenous Australians minus the age-standardised rate (per 100,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D1.18.24. AIHW National Mortality Database.
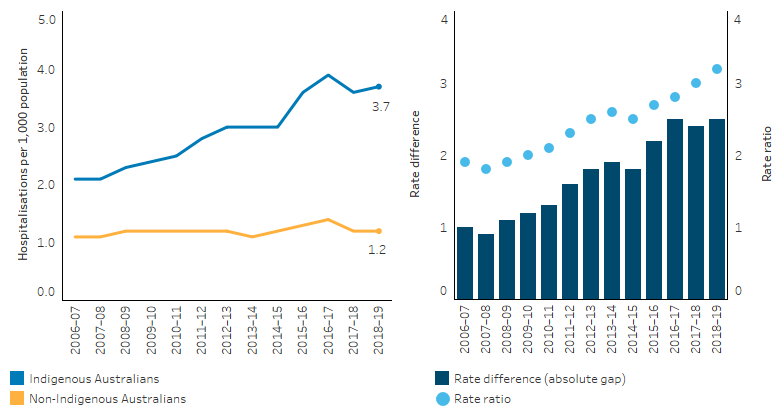
Between 2009–10 and 2018–19, there was a 52% increase in the hospitalisation rate (from 19 to 29 hospitalisations per 1,000 population, crude rates) for mental health-related conditions (based on principal diagnosis), with a higher increase for Indigenous females (58%; from 18 to 29 per 1,000), than Indigenous males (46%; from 20 to 30 per 1,000). These data are for six jurisdictions combined where the quality of Indigenous status information is considered of adequate quality over the time period considered (New South Wales, Victoria, Queensland, Western Australia, South Australia and the Northern Territory).
Based on age-standardised rates, between 2009–10 and 2018–19, the rate of hospitalisations for mental health-related conditions (based on principal diagnosis) for Indigenous Australians increased by more than for non-Indigenous Australians (increasing by 52% compared with by 30%). This resulted in a widening of the absolute gap (rate difference) over the period.
The relative difference between the two populations was 1.4 times the rate of non-Indigenous Australians in 2009–10, compared with 1.9 times the rate of non-Indigenous Australians in 2018–19 (Table D1.18.20, Figure 1.18.8).
Figure 1.18.8: Age-standardised hospitalisation rates for mental health-related conditions as principal diagnosis, by Indigenous status, NSW, Vic, Qld, WA, SA and NT 2006–07 to 2018–19
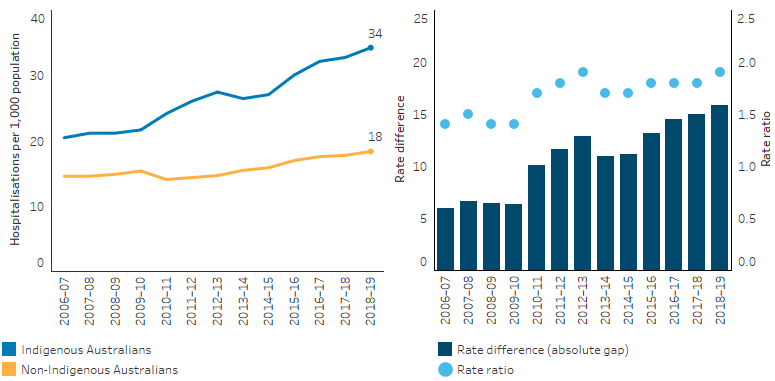
Notes
1. The care type Mental health was introduced from 1 July 2015. To change the care type of patients receiving mental health care, Queensland (in 2015–16) and New South Wales (in 2016–17) discharged and readmitted patients, causing the rise in hospitalisations and patient days counted in those years.
2. Rate difference is the age-standardised rate (per 1,000) for Indigenous Australians minus the age-standardised rate (per 1,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D1.18.20. AIHW analysis of National Hospital Morbidity Database.
From 2009–10 to 2018–19, there was an overall 63% increase in the rate of hospitalisations due to intentional self-harm for Indigenous Australians (from 2.3 to 3.6 hospitalisations per 1,000 population). The rate increased by 75% for Indigenous females (from 2.6 to 4.4 hospitalisations per 1,000) and increased by 43.4% for Indigenous males (from 2.0 to 2.7 per 1,000). This was for the six jurisdictions with Indigenous identification data of adequate quality (New South Wales, Victoria, Queensland, Western Australia, South Australia and the Northern Territory).
After adjusting for differences in the age structure between the two populations, the relative difference between the two populations increased. The rate for Indigenous Australians was twice the rate of non-Indigenous Australians in 2009–10 and increased to 3.2 times the rate of non-Indigenous Australians in 2018–19 (Table D1.18.29, Figure 1.18.9).
Figure 1.18.9: Age-standardised hospitalisation rates for injury and poisoning (based on principal diagnosis) with a first reported external cause of self-harm, by Indigenous status, NSW, Vic, Qld, WA, SA and NT, 2006–07 to 2018–19
Note: Rate difference is the age-standardised rate (per 1,000) for Indigenous Australians minus the age-standardised rate (per 1,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D1.18.29. AIHW analysis of National Hospital Morbidity Database.
Research and evaluation findings
Protective factors and healing
Drawing on data from four ABS health and social surveys: National Aboriginal and Torres Strait Islander Social Survey (NATSISS) 2002 and 2008, and National Aboriginal and Torres Strait Islander Health Survey (NATSIHS) 2004–05 and 2012–13, employment status and housing tenure were shown to be significantly associated with a range of health and wellbeing outcomes. A range of health and wellbeing indicators were assessed: self-assessed health, having specific health issues (i.e., asthma, and heart or cardiovascular (circulatory) problems or diseases), emotional wellbeing (measured by Kessler-5 and subjective feelings of happiness and sadness) and tobacco and alcohol use. Indigenous Australians who were employed had better health and wellbeing outcomes compared with those who were unemployed across surveys conducted between 2002 and 2013. Indigenous Australians who were renting had lower health and wellbeing outcomes compared with Indigenous property owners. As education levels have increased for Indigenous Australians, the association of education with health and wellbeing has weakened (Crawford & Biddle 2017).
Research into the impact of stigma and discrimination related to problematic alcohol and other drug use in Queensland found that participants ‘felt their best when connected to their families and communities, and when being noticed, respected and cared for’, and when they were able to support others (QMHC 2020). Employment and education were seen as drivers of good mental health and wellbeing.
A review of research focused on Indigenous peoples from Canada, Australia, New Zealand and the United States (CANZUS nations) found that culture is significantly and positively associated with physical health, social and emotional wellbeing, and reduces risk-taking behaviours (Bourke et al. 2018). Across the literature there were conceptual variations in defining and measuring culture. Cultural domains, including language, cultural expression and connection to country were more likely to be reported in quantitative studies, and cultural domains of knowledge, beliefs, kinship, and family were more likely to be reported using qualitative methods.
A systematic review of programs that include components to enable and support Indigenous Australians to express cultural identity found that such programs can have positive health and wellbeing effects, including on mental health and reducing substance use (MacLean et al. 2017). Research conducted with Indigenous children living on the South Coast of New South Wales found that positive emotional wellbeing was an outcome of connecting Indigenous children to cultural practices, and cultural interactions gave children a sense of identity and belonging (Crowe et al. 2017). Healthy lifestyle behaviours related to physical activity and healthy eating were interconnected with cultural practices.
A systematic review of evaluated resilience-enhancing interventions conducted in, or in partnership with, schools for Indigenous adolescents in the CANZUS nations, found that some interventions focused on fostering individual resilience only; others included aspects intended to build staff, school and/or community capacity to support adolescent resilience; and several had community/school capacity building as the primary focus (Jongen et al. 2019). Approaches based on culture were present in most studies. The evaluations described in the review found a range of positive outcomes, with the most common being in the resilience of participating adolescents, such as coping skills and communication/conflict resolution skills. Improvements in mental health-related outcomes were also evident, such as reduced substance use.
Indigenous Ranger programs generate employment opportunities for Indigenous Australians, and improve biodiversity and land management outcomes (Jones et al. 2018). The work of Indigenous rangers is highly valued by Indigenous communities across Australia, for achieving both environmental and employment outcomes, alongside wider social, cultural and economic benefits. An independent evaluation of the Indigenous Rangers and Indigenous Protected Areas programs in 2016 found that rangers had experienced increased confidence and skills through their training and work on country (PM&C 2019). Participation in Ranger programs facilitates cultural engagement through caring for country and transfer of customary ecological knowledge and practices. Research using data collected in Central Australia in 2017 through field testing of the Mayi Kuwayu Study (The National Study of Aboriginal and Torres Strait Islander Wellbeing) compared life satisfaction, general health, psychological wellbeing and family wellbeing among 43 Indigenous Australians employed as Rangers, compared with 160 Indigenous Australians who were not employed as Rangers. The study found, after adjusting for employment, income, education, health risk factors and conditions, that Ranger participation was strongly associated with very high life satisfaction and high family wellbeing, but did not identify an association with psychological wellbeing. These findings support assertions from communities, Indigenous organisations and conservation groups that the Indigenous Ranger program is contributing towards closing gaps in health, employment and education. The study suggests that stability and expansion in policies that facilitate the development, implementation and sustainability of Ranger programs are likely to lead to improved wellbeing, health, and other gains for Indigenous Australians.
Indigenous women and girls possess social and cultural strengths which can be drawn on to drive local action as natural leaders and role-models. Dudgeon and Bray (2018) found that Indigenous Australian women’s social and emotional wellbeing has been affected by the impact of colonisation and past policies such as the forced removal of children. However, Indigenous Australian women have maintained strong leadership roles and have kept families and communities together. In recent decades Indigenous mental health and self-determination have become more prominent movements, restoring and strengthening the role women have in traditional healing practices (Dudgeon & Bray 2018). Ngangkari traditional women healers are ‘leading a renaissance of cultural healing’ and are focused on a ‘restorative, holistic decolonisation of people’s social and emotional wellbeing’. The Ngaanyatjarra Pitjantjatjara Yankunytjatjara Women’s Council employs Ngangkari healers to work in communities in the region, and in hospitals, nursing homes, hostels, health services and prisons in regional centres (Hawthorne 2018). Traditional healing has been recognised as an important and effective intervention into the transmission of intergenerational trauma (Dudgeon & Bray 2018). Traditional healers play an important role in the healing process for Indigenous Australians and influence and support the positive management of Indigenous Australians’ emotional, spiritual and physical wellbeing. ‘Building access to cultural healers and cultural healing across all parts of the Australian mental health system’ for Indigenous Australians was identified as a key element for implementing the Gayaa Dhuwi (Proud Spirit) Declaration, which proposes that change is needed across all levels of the mental health system (Dudgeon et al. 2016a).
Aboriginal and Torres Strait Islander Mental Health First Aid (MHFA) Training delivered to Groote Eylandt and Bickerton Island between December 2016 and May 2017 was evaluated (NIAA 2019). Participant feedback indicated that the training was highly relevant, and 85% thought they would need to use their new skills in the next 12 months. The evaluation found the training was effective in increasing the ability of participants to recognise the signs of mental health issues, and increasing their knowledge of how to implement the MHFA action plan including how to approach, assess and assist with any mental health crisis.
Life stressors
Colonisation disrupted sources of social and emotional wellbeing within cultures, communities and families, with resulting intergenerational impacts (Calma et al. 2017). These effects are exacerbated by the negative impact of social determinants today, including the forced removal of children from families, racism and broader forms of social exclusion. Addressing these social determinants requires a collaborative approach that includes services outside the health sector, including housing, education, employment, recreation, child protection and family services, crime prevention and justice (Commonwealth of Australia 2017).
A demographic assessment of life outcomes facing Stolen Generations survivors and their descendants used ABS Aboriginal and Torres Strait Islander Health and Social Survey data to identify individuals who were born before 1972 and who reported being removed from their families (AIHW 2018, 2021). Compared with other older Indigenous Australians who did not report having been removed, the Stolen Generations aged 50 years and over were found to have poorer outcomes across a range of indicators, including health status, income and employment status, home ownership, experiences of discrimination, access to services, and contact with police and the criminal justice system. Stolen Generations survivors were more likely to be living with ill health and other stressors compared with other older Indigenous Australians, including, for example, to experience discrimination due to being Indigenous, to experience actual or threatened violence, to have a disability, to have poorer mental health or to have been diagnosed with a mental health condition (AIHW 2021). The Healing Foundation designs projects that encourage collective healing, where people are supported and empowered to heal through group activities such as gatherings and family reunions (The Healing Foundation). This is particularly important for Stolen Generations survivors who were institutionalised and had connections with land and culture damaged. In addition, Link Up Services provide family tracing, reunion and support services to Stolen Generations members. Stolen Generations members can also access a range of social and emotional wellbeing services which provide practical supports such as individual counselling, case management, group therapy, community engagement, outreach, family support, group and community healing activities.
Research in the Northern Territory has found a significant association between interpersonal racism and depression among Indigenous Australians after adjusting for sociodemographic factors. Lack of control, stress, negative social connections and reactions to racism such as feeling ashamed or powerless were each identified in the relationship between racism and depression (Paradies & Cunningham 2012). A study of 755 Indigenous Australian Victorians also found an association between reported racism and psychological distress (Kelaher et al. 2014). Community consultations in Queensland outlined the profound impact that racism, discrimination and negative stereotypes had on participants’ social and emotional wellbeing (QMHC 2020).
‘Lateral violence’ affects Indigenous peoples all around the world, and stems from the sense of powerlessness that comes from oppression, where members of an oppressed group direct their fear and anger toward each other, and toward those less powerful than themselves (see measure 2.10 Community safety) (AHRC 2011). The ways in which lateral violence can affect social and emotional wellbeing are multilayered and vary based on each person’s strengths and risk factors. This effect is subtly different from other forms of bullying and violence, as it can ‘undermine cultural identity’ and ‘devalue pride in culture and self-worth’. Cultural safety and cultural security help create positive and empowered environments where the problems of lateral violence can be solved. An Adelaide study conducted interviews with 30 Indigenous Australians about their experience of lateral violence and coping strategies (Clark et al. 2016, 2017). The study found that many participants with high psychological distress had experienced lateral violence, but also that they identified strategies to handle and prevent it. The study found education and awareness was the strategy most raised by participants, but also noted the need for a variety of legal, workplace and cultural support. Cultural renewal programs aim to prevent lateral violence by increasing connection to and pride in culture (AHRC 2011). Empowerment is also important because historical and continuing disempowerment breeds lateral violence. Solutions to lateral violence must come from within Indigenous communities as they exercise their right to self-determination. Governments can assist by removing the obstacles that prevent communities from taking control, and by helping build capacity within communities so they are able to take on these responsibilities.
Family violence has a profound effect on social and emotional wellbeing. Family violence, including gender-based violence, places a huge burden on Indigenous communities, especially women and children (Closing the Gap Clearinghouse 2016) (see measure 2.10 Community safety). Family violence is not part of Indigenous culture. Culture and family are key protective factors that support communities to be free of violence. Discrimination, racism and intergenerational trauma are some of the significant drivers that impact Indigenous Australians.
Breaking the cycle of violence requires community-driven, healing aware and trauma informed approaches to family violence that prioritise local needs, cultural healing, family restoration and the strengths of Indigenous families. Indigenous-led solutions must support frontline and preventive services, as well as the structural drivers of violence. Programs showing promising results include the Maranguka Justice Reinvestment Project in Bourke, a model of Indigenous self-governance where an Indigenous community owned and led multi-disciplinary team works in partnership with government and non-government agencies (AIHW 2019; Just Reinvest NSW Inc.). The project is guided by the Bourke Tribal Council, comprising representatives from the different Tribal Groups living in Bourke (Just Reinvest NSW Inc. ; KPMG Australia & Just Reinvest NSW Inc. 2018). Maranguka, meaning ‘caring for others’ in Ngemba language, has delivered a number of interlinked activities designed to create impact at different levels of the community and justice system (KPMG Australia & Just Reinvest NSW Inc. 2018). Activities include the Indigenous leadership driving a grassroots movement for change among local community members; facilitating collaboration and alignment across the service system; delivering new community-based programs and service hubs; and working with justice agencies to evolve their procedures and behaviours towards a proactive and reinvestment model of justice. Maranguka has successfully demonstrated reductions in police-reported family violence incidents and improvements in community safety indicators (AIHW 2019; KPMG Australia & Just Reinvest NSW Inc. 2018).
The National Empowerment Project (NEP) was a universal strategy to promote social and emotional wellbeing and reduce community distress and suicide in Aboriginal and Torres Strait Islander communities, and funded by the Australian Government under the National Mental Health Program. The project set out to consult with 457 people in 11 communities across Australia to understand the challenges that are causing psychological distress and high rates of suicide in Aboriginal and Torres Strait Islander communities. During the NEP consultations, communities also stated that culture is a significant factor in social and emotional wellbeing. This led to the adoption of the term Cultural, Social, and Emotional Wellbeing (CSEWB). The program was initially delivered in two Queensland communities: Kuranda and Cherbourg between 2014 and 2016 (Mia et al. 2017). The CSEWB program aimed to promote positive cultural, social and emotional wellbeing and mental health, build resilience and prevent psychological distress and suicide, and address community identified problems such as family violence and substance misuse that were contributing to high levels of suicide and family and community issues in the two communities. The CSEWB program was Indigenous-led, needs-based and strengthened by involving local communities and local community co-researchers in consultation, design, implementation and evaluation of the program. Considerable work was undertaken prior to program implementation to ensure community readiness and ownership. An evaluation of the CSEWB program collected information from program participants through interviews, ‘Stories of Most Significant Change’ and a review of NEP site reports. Several female participants said the program provided them with skills to more successfully deal with family and domestic violence and family breakdown, and commit to a stronger resolve to address these issues and make better life choices for themselves, their children, and families. Interviews with participants described how the CSEWB program had significantly changed their lives and their families’ lives in various constructive and affirming ways to bring about positive outcomes. The 2017 evaluation report identified that the CSEWB program contributed to healing among families, strengthening role models for future generations, and reaffirming cultural identity in the participants and their communities (Mia et al. 2017). The program was also delivered in Western Australia by the Langford Aboriginal Association in three communities: Langford, Kwinana and Girrawheen (Perth metropolitan regions). The 2019 evaluation report reaffirmed the importance of culturally safe programs that acknowledge historical and social determinants of health at both local and national levels (The National Empowerment Project 2019). The program evaluation provided strong evidence for the importance of relational and holistic models of health for healing and empowerment for Aboriginal and Torres Strait Islander people.
Social and emotional wellbeing of children and young people
In the Longitudinal Study of Indigenous Children (LSIC), primary carers were asked whether the child participating in LSIC had been bullied or treated unfairly at preschool or school by children or adults because they are Indigenous. Research using the LSIC found that racial discrimination places Indigenous children at a moderately increased risk of negative mental and physical health outcomes, and that age of first exposure did not have a consistently greater impact across outcomes (Cave et al. 2019). However, a stronger adverse effect was found on behavioural issues for first exposure at 7 years relative to 4–5 years, and on mental health for first exposure at 4–5 years relative to 7 years. A separate analysis found that Indigenous children participating in the LSIC who had been exposed to racism had an increased risk of emotional and behavioural difficulties (Macedo DM et al. 2019a). Another research project using the LSIC found that more than 43% of Indigenous children aged 6–10 years had six or more risk factors for mental illness in adulthood, and 23% were experiencing current psychological distress (Twizeyemariya et al. 2017). The study found that substantial risk was present from infancy, with 67% of Indigenous children aged 0–1 years exposed to three or more major life events. However, despite high levels of adversity, the children participating in the LSIC generally reported a positive sense of self, suggestive of resilience. Other research has shown that Indigenous children in LSIC who experienced more major life events had a higher risk of experiencing social and emotional difficulties, and that good mental health of the primary carer was a protective buffer for children experiencing major life events (FaHCSIA 2015; Salmon et al. 2018). Macedo et al. (2019) found that ‘ethnic-racial identity’ affirmation had a protective effect on Indigenous children in the LSIC who had been exposed to racism, while children with low ethnic-racial identity affirmation, whose parents reported they experienced discrimination/racism, were at increased risk of poor social and emotional wellbeing two years later (Macedo Davi M et al. 2019b). The report A Decade of Data: Findings from the first 10 years of Footprints in Time shows the importance of LSIC parents’ social and emotional wellbeing for children’s learning, psychological distress and children’s social and emotional wellbeing (Department of Social Services 2020; Thurber et al. 2019).
Research has shown that parental stress caused by factors such as unemployment and financial problems is associated with emotional or behavioural difficulties in children and decreased utilisation of health services for the child's needs (Ou et al. 2010; Strazdins et al. 2010).
The Study of Environment on Aboriginal Resilience and Child Health (SEARCH) is a large-scale cohort study in New South Wales, which aims to identify the determinants and trajectories of health in urban Indigenous children and their caregivers, conducted in partnership with four Aboriginal Community Controlled Health Services. Phase one was conducted over the period 2006 to 2012, involving 1600 Indigenous children and their caregivers. Research drawn from Phase one studied findings of 119 Indigenous teenagers living in urban areas, using a Strengths and Difficulties Questionnaire to measure resilience (Young et al. 2019). The study found that most Indigenous adolescent participants displayed resilience, while 16% were at high risk of clinically significant behavioural and emotional problems. Greater resilience was associated with nurturing family environments, social support and regular exercise.
A 2013 review of research, policies and programs addressing the social and emotional wellbeing of Indigenous youth found that there is a need for greater recognition of the extreme circumstances many Indigenous youth grow up within, and that successful ways forward require strengths-based holistic approaches that promote cultural identity (Haswell et al. 2013).
A 2013 evaluation of a Brisbane headspace social and emotional wellbeing group-based program examined two-month follow up data available for 49 Indigenous youth participants aged 11–21 years (Skerrett et al. 2018). The evaluation found a decrease in suicidal ideation and indications that participants improved their understanding of holistic health and had an increased number of coping skills.
The save-a-mate (SAM) Our Way program was evaluated in 2012, and was operating in 14 sites across the Northern Territory, Queensland, South Australia, and Western Australia at the time (Blignault et al. 2016). The program’s broad aim was to improve the social and emotional wellbeing of young Indigenous Australians, with a focus on depression, anxiety, violence and alcohol and other drug problems, by engaging young people and strengthening stakeholder and community responses to wellbeing issues affecting Indigenous youth. The program took a community development approach based on culturally respectful ways of working and partnerships with Indigenous communities. The evaluation found a tension between community development and specific program delivery, and that program staff at each site learned not to be too ambitious, and to work consistently with the community to establish partnerships, gain trust and engage and train community members.
The Youth Empowerment and Healing Cultural Camp in Western Australia run one-week camps for children and youth at risk of suicide or who have had first-hand experience of suicide. The community-led and directed program aims to strengthen wellbeing and resilience through social empowerment and healing by providing connection to culture and country. Participants learn about sharing, caring and community values through greater connection to culture and country. An internal evaluation of the program showed that participants reported being better able to deal with challenging feelings after attending the camp (Shadforth & Shadforth 2018). The Centre for Best Practice in Aboriginal and Torres Strait Islander Suicide Prevention (CBPATSISP) assessed the program as strong evidence of effectiveness, commitment and alignment to CBPATSISP best practice principles ((Shadforth & Shadforth 2018; The Centre for Best Practice in Aboriginal and Torres Strait Islander Suicide Prevention 2022).
Intentional self-harm and suicide
A literature review on protective and risk factors for suicide among Indigenous Australians summarised findings from 214 reports, research articles and systematic reviews, and concluded 17 critical protective and risk factors associated with an individual’s intention to suicide. Factors that affect both Indigenous and non-Indigenous Australians include: age, sex, location of residence, housing, employment, substance use and incarceration. The review also highlights the unique factors that may be particularly important Indigenous Australians: cultural continuity, spirit, language and cultural understandings of wellbeing (AIHW 2022b).
Based on consultation and research, a report by the AIHW sought to further understand the sources of data that can inform progress to reduce Aboriginal and Torres Strait Islander suicide, supporting the need for accurate and timely data about Indigenous suicide deaths and non-lethal intentional self-harm (AIHW 2022a). The report:
- Provides a detailed description of the key players and stages in the identification and recording of suicide and non-lethal intentional self-harm incidents among Aboriginal and Torres Strait Islander people.
- Brings together information on suicide-relevant data collections with national, state or territory coverage: including their purpose; their Indigenous status derivation; and their limitations.
- Identifies the sources of error in the classification of Indigenous status; of suicide as a cause of death; and of suicidal intent in cases of self-harm.
- Describes the work already underway to enhance the quality, consistency and timeliness of data collection and reporting, and work that needs to be undertaken (AIHW 2022a).
A study of emergency department presentations at the Alice Springs Hospital and Royal Darwin Hospital in the Northern Territory reviewed 167 presentations involving suicide-related thoughts and behaviours over a two month period in 2013 (Leckning et al. 2020). Indigenous patients were more likely than non-Indigenous patients to present from remote areas and to report substance misuse and family conflict or violence. In both groups, males were more likely than females to be admitted, and people presenting with self-harm were more likely to be admitted than those who had suicidal thoughts only. The study did not identify any differences in discharge arrangements by Indigenous status. Exposure to family conflict or violence is strongly indicative of the effects of intergenerational trauma on community and family functioning that increases the likelihood of psychological distress. Family and community are also an important source of identity and social and emotional wellbeing, protective factors against suicide-related thoughts and behaviours. An understanding of family relationships can assist with ‘appropriate assessment of individual and contextual risk and sources of cultural strengths and resilience’ to help ensure decisions about aftercare for Indigenous patients lead to appropriate and safe support.
High Indigenous suicide rates arise from a complex web of interacting personal and social circumstances (Dudgeon et al. 2017). A history of colonisation, burden of intergenerational trauma, and contemporary disadvantage and discrimination can impact on potential sources of social and emotional wellbeing and resilience that help protect Indigenous people against suicide. Indigenous Australians’ greater exposure to life stressors, traumatic events, passing away of family members and friends, attendance at grieving rituals and associated drug and alcohol use are also factors. Cultural education, cultural reclamation activities and cultural continuity have a significant role to play in Indigenous suicide prevention, particularly for young people.
A systematic review found that Indigenous youth in Australia have elevated rates of suicide, self-harm and suicidal ideation (Dickson et al. 2019). Risk factors included being incarcerated, substance use and greater social and emotional distress. The review found there was a scarcity of information on predictors of suicide and self-harm (Dickson et al. 2019). High rates of non-fatal intentional injury are an important focus for preventive and early intervention (Azzopardi et al. 2018).
National Coronial Information System data have shown that between 2001 and 2017, young people aged under 25 identifying as Aboriginal and/or Torres Strait Islander comprised 12.9% (738) of youth self-harm deaths. Indigenous youth self-harm deaths were more likely to be younger, female and unemployed than their non-Indigenous counterparts (National Coronial Information System 2020).
An audit of reported suicide deaths provided to the Kimberley Mental Health and Drug Service for the period 2005–2014 found that Indigenous suicide rates in the Kimberley region had dramatically increased over the decade, with an overall trend upwards in youth suicides and female suicides (Campbell et al. 2016). A study in Western Australia found that Indigenous mothers were 3.5 times as likely to commit suicide as non-Indigenous mothers (Fairthorne et al. 2016).
A coronial inquest into 13 deaths of children and young people in the Kimberley that occurred from 2012 to 2016 found that 12 occurred by way of suicide (Fogliani 2019). The coroner found that individual events were shaped by the effects of intergenerational trauma and poverty upon entire communities. The coroner’s report made 42 recommendations including improved screening and services for people with fetal alcohol spectrum disorder; restrictions on take away alcohol; the appointment of a Commissioner for Indigenous children and youth; and that emphasis be given to principles of self-determination and empowerment in policies and programs relating to Indigenous Australians in Western Australia, with measures introduced to facilitate their involvement. The report acknowledged the considerable services being provided to the region, but concluded that they were insufficient and provided by mainstream services that were attempting to adapt in culturally relevant ways. The coroner recommended consideration of services being co-designed, with ‘a more collective and inclusive approach towards cultural healing’. The 2016 Message Stick Inquiry found that Indigenous youth suicide is indicative of a distressed community and that effective solutions must be community focused (Education and Health Standing Committee 2016). The Government of Western Australia’s response to the coroner’s inquest and the Message Stick report was released in March 2020 (Government of Western Australia 2020).
The Coroners Court of Victoria (2020) released a report on suicides of Indigenous Australians in Victoria, prepared by the Coroners Koori Engagement Unit and Coroners Prevention Unit (Coroners Court of Victoria 2020). The report found that between 1 January 2009 and 30 April 2020, there were 117 suicides of Indigenous Australians in Victoria. Of these 82 were male and 35 were female. Over half (59.8%) of the suicides occurred in Regional Victoria, with 40.2% occurring in Metropolitan areas of Victoria. Indigenous Australian Victorians had experienced higher rates of contact with the legal system (Police, Courts and Corrections) within six weeks and within 12 months prior to suicide, compared with all Victorians. Substance use and misuse was identified as a contextual stressor in 82.6% of suicides of Indigenous Victorians, and experience of abuse (either as the perpetrator or the victim) in 63.8% of suicides. Interpersonal stressors were identified in around two-fifths of suicides of Indigenous Victorians, described as conflict with partner (44.9%), conflict with family members (43.5%), family violence with partner, either as the perpetrator or the victim (36.2%) and separation from partner (47.8%). The report notes that due to the low frequency of suicides, the data must be interpreted with caution.
Implications
The policy responses to social and emotional wellbeing need to be multidimensional and involve a wide range of stakeholders. It is paramount that strategies build on the strengths, resilience and endurance within Indigenous communities and recognise the important historical and cultural diversity within communities (Dudgeon et al. 2014; Social Health Reference Group 2004). Suicide prevention studies have identified the need to focus on protective factors, such as community connectedness, strengthening the individual and rebuilding family, as well as culturally based programs (AIHW & AIFS 2013; Clifford et al. 2012; Cox et al. 2014; Dudgeon et al. 2012; Ridani et al. 2015; Tighe & McKay 2012). Approaches to suicide prevention should be Indigenous-led, and include healing activities and support to address community challenges, including the use of community support people. The increasing Indigenous suicide rate suggests that current approaches to Indigenous suicide prevention are not yet effective (Dudgeon et al. 2017). To support access to mental health services for Indigenous Australians it is important for all mental health services to offer a culturally safe environment (see measure 3.10 Access to mental health services). Culturally valid understandings must shape the provision of services and guide assessment, care and management of Indigenous Australians’ health (Department of Health 2017). Mental health services staff working with Indigenous Australians at risk of suicide and in Indigenous communities should demonstrate cultural competence and provide trauma informed care (Dudgeon et al. 2016b). Guidelines have been developed for best practice assessment of Indigenous Australians presenting with self-harm or suicidal thoughts at hospitals (Leckning et al. 2019).
Addressing the needs of Indigenous youth in particular, requires investment and actions in sectors that extend beyond health (Azzopardi et al. 2020). For example, the education sector provides an important platform for building Indigenous youth wellbeing and resilience, and opportunities for early intervention and prevention, and it is important that education is culturally safe and responsive to the needs arising from socioeconomic inequity, insecure housing, teenage parenthood and poor physical and mental health.
The Indigenous Advancement Strategy’s Safety and Wellbeing Programme provides funding to a range of social and emotional wellbeing services and workforce support, Aboriginal and Torres Strait Islander Mental Health First Aid and the National Indigenous Postvention Service, to enhance community safety and support Indigenous wellbeing.
The National Strategic Framework for Aboriginal and Torres Strait Islander Peoples’ Mental Health and Social and Emotional Wellbeing 2017–2023 provides a dedicated focus on Aboriginal and Torres Strait Islander social and emotional wellbeing and mental health and sets out a comprehensive and culturally appropriate stepped care model that is applicable to both Indigenous specific and mainstream health services. The Framework is designed to complement the Fifth National Mental Health and Suicide Prevention Plan (the Fifth Plan), endorsed in 2017. The Fifth Plan seeks to establish a national approach for collaborative government effort from 2017–2022 across eight targeted priority areas, including improving Indigenous Australian mental health and suicide prevention. More information on the Framework, Fifth Plan and the Implementation Plan for the Fifth Plan is in <Policies and Strategies>.
The National Mental Health and Suicide Prevention Agreement (the Mental Health Agreement) sets out the shared intention of the Commonwealth, state and territory governments to work in partnership to improve the mental health of all Australians and ensure the sustainability and enhance the services of the Australian mental health and suicide prevention system. The Mental Health Agreement aims to achieve systemic, whole-of-government reform to deliver a comprehensive, coordinated, consumer-focused mental health and suicide prevention system with joint accountability across all governments. The Mental Health Agreement commits to continuing work under the Fifth Plan and responds to the recommendations of the Productivity Commission Inquiry into Mental Health, the National Suicide Prevention Adviser’s Final Advice, and the House of Representatives Select Committee on Mental Health and Suicide Prevention Final Report. The priority areas addressed within the Mental Health Agreement include regional planning and commissioning, priority populations, stigma reduction, safety and quality, gaps in the system of care, suicide prevention and response, psychosocial supports outside the National Disability Insurance Scheme (NDIS), national consistency for initial assessment and referral, workforce, and data and evaluation. The Mental Health Agreement identifies Aboriginal and Torres Strait Islander peoples as a priority population, and commits to work in partnership with Indigenous Australians, their communities, organisations and businesses to improve their access to, and experiences of, social and emotional wellbeing, and mental health and suicide prevention services. The Mental Health Agreement is supported by bilateral schedules with all states and territories. Bilateral schedules outline funding commitments to deliver specific initiatives at a state-level and allow for regional variability in the delivery of those initiatives. The Mental Health Agreement and bilateral schedules are publicly available on the Federal Financial Relations Website.
The Indigenous Mental Health and Suicide Prevention Clearinghouse was established to build the evidence base to improve mental health services and outcomes for Indigenous Australians. It includes an exploration of mental health and suicide related topics, research articles, and a research and evaluation register.
The National Agreement on Closing the Gap was developed in partnership between Australian governments and the Coalition of Aboriginal and Torres Strait Islander Peak Organisations. The National Agreement has been built around four Priority Reforms that will change the way governments work with Indigenous Australians. These reforms outline obligations for governments to work in partnership; share decision making; build the community controlled sector; transform government organisations; and provide shared access to regional level data. Priority Reform Three in particular, has implications for the way mainstream services need to transform to eliminate racism and deliver culturally safe services that are responsive to the needs of Indigenous Australians.
The policy context is at Policies and strategies.
References
-
Aboriginal and Torres Strait Islander Healing Foundation 2021. Impacts of COVID-19 on Stolen Generations survivors. Canberra: Aboriginal and Torres Strait Islander Healing Foundation.
-
ABS (Australian Bureau of Statistics) 2016. National Aboriginal and Torres Strait Islander Social Survey 2014–15. Cat. no. 4714.0. Canberra.
-
ABS 2019. National Aboriginal and Torres Strait Islander Health Survey, 2018–19. 4715.0. Canberra: ABS.
-
AHRC (Australian Human Rights Commission) 2011. Social Justice Report 2011. Sydney: AHRC.
-
AIHW (Australian Institute of Health and Welfare) 2014. Determinants of wellbeing for Indigenous Australians. Cat. no. IHW 137. Canberra: AIHW.
-
AIHW 2018. Aboriginal and Torres Strait Islander Stolen Generations and descendants: numbers, demographic characteristics and selected outcomes. Canberra: AIHW.
-
AIHW 2019. Family, domestic and sexual violence in Australia: continuing the national story 2019. Canberra: AIHW.
-
AIHW 2021. Aboriginal and Torres Strait Islander Stolen Generations aged 50 and over: updated analyses for 2018–19. Cat. no. IHW 257. Canberra: AIHW.
-
AIHW 2022a. Investigating enhancements of Indigenous data in suicide-relevant data sets. Canberra: AIHW.
-
AIHW 2022b. Protective and risk factors for suicide among Indigenous Australians. Canberra: AIHW: AIHW, Australian Government.
-
AIHW 2022c. Australian Burden of Disease Study: Impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018. Canberra: AIHW.
-
AIHW & AIFS (Australian Institute of Health and Welfare & Australian Institute of Family Studies) 2013. Strategies to minimise the incidence of suicide and suicidal behaviour. Canberra: AIHW.
-
Australian Psychological Society 2018. Accessibility and quality of mental health services in rural and remote Australia APS response to the Senate Community Affairs References Committee Inquiry - Submission 103.
-
Azzopardi P, Blow N, Purcell T, Brown N, Ritchie T & Brown A 2020. Investing in the health of Aboriginal and Torres Strait Islander adolescents: a foundation for achieving health equity. Medical Journal of Australia 212:202–4. e1.
-
Azzopardi P, Sawyer S, Carlin J, Degenhardt L, Brown N, Brown A et al. 2018. Health and wellbeing of Indigenous adolescents in Australia: a systematic synthesis of population data. The Lancet 391:766–82.
-
Blignault I, Haswell M & Pulver LJ 2016. The value of partnerships: lessons from a multi‐site evaluation of a national social and emotional wellbeing program for Indigenous youth. Australian and New Zealand journal of public health 40:S53–S8.
-
Bourke S, Wright A, Guthrie J, Russell L, Dunbar T & Lovett R 2018. Evidence Review of Indigenous Culture for Health and Wellbeing. International Journal of Health, Wellness & Society 8.
-
Calma T, Dudgeon P & Bray A 2017. Aboriginal and Torres Strait Islander social and emotional wellbeing and mental health. Australian Psychologist 52:255–60.
-
Campbell A, Chapman M, McHugh C, Sng A & Balaratnasingam S 2016. Rising Indigenous suicide rates in Kimberley and implications for suicide prevention. Australasian Psychiatry 24:561–4.
-
Cave L, Shepherd CC, Cooper MN & Zubrick SR 2019. Racial discrimination and the health and wellbeing of Aboriginal and Torres Strait Islander children: Does the timing of first exposure matter? SSM-population health 9:100492.
-
Clark Y, Augoustinos M & Malin M 2016. Lateral violence within the Aboriginal community in Adelaide:“It affects our identity and wellbeing”. Journal of Indigenous Wellbeing 1:43–52.
-
Clark Y, Augoustinos M & Malin M 2017. Coping and prevention of lateral violence in the Aboriginal community in Adelaide. Australian Community Psychologist 28:105–23.
-
Clifford A, Doran CM & Tsey K 2012. Suicide prevention interventions targeting Indigenous peoples in Australia, New Zealand, the United States and Canada: a rapid review. Sax Institute.
-
Closing the Gap Clearinghouse 2016. Family violence prevention programs in Indigenous communities. Vol. Resource sheet no. 37. Produced by the Closing the Gap Clearinghouse Canberra: Australian Institute of Health and Welfare, Melbourne: Australian Institute of Family Studies.
-
Commonwealth of Australia 2017. National Strategic Framework for Aboriginal and Torres Strait Islander Peoples’ Mental Health and Social and Emotional Wellbeing 2017-2023. Canberra: Department of the Prime Minister and Cabinet.
-
Coroners Court of Victoria 2020. Victorian suicides of Aboriginal and Torres Strait Islander people.
-
Cox A, Dudgeon P, Holland C, Kelly K, Scrine C & Walker R 2014. Using participatory action research to prevent suicide in Aboriginal and Torres Strait Islander communities. Australian journal of primary health 20:345–9.
-
Crawford H & Biddle N 2017. Changing associations of selected social determinants with Aboriginal and Torres Strait Islander health & wellbeing, 2002 to 2012-13, Working Paper No. 113/2017. Canberra: CAEPR.
-
Crooks K, Casey D & Ward J 2020. First Nations people leading the way in COVID-19 pandemic planning, response and management. Medical Journal Australia.
-
Crowe R, Stanley R, Probst Y & McMahon A 2017. Culture and healthy lifestyles: a qualitative exploration of the role of food and physical activity in three urban Australian Indigenous communities. Australian and New Zealand journal of public health 41:411–6.
-
Department of Health (Australian Government Department of Health) 2017. My Life My Lead - Opportunities for strengthening approaches to the social determinants and cultural determinants of Indigenous health: Report on the national consultations. Canberra: Department of Health.
-
Department of Health 2020. Australian Health Sector Emergency Response Plan for Novel Coronavirus (Covid-19). Canberra: Department of Health.
-
Department of Social Services 2020. A Decade of Data: Findings from the first 10 years of Footprints in Time. Canberra: DSS.
-
Dickson JM, Cruise K, McCall CA & Taylor PJ 2019. A systematic review of the antecedents and prevalence of suicide, self-harm and suicide ideation in Australian Aboriginal and Torres Strait Islander youth. International journal of environmental research and public health 16:3154.
-
Dudgeon P & Bray A 2018. Indigenous healing practices in Australia. Women & Therapy 41:97–113.
-
Dudgeon P, Calma T, Brideson T & Holland C 2016a. The Gayaa Dhuwi (Proud Spirit) Declaration–a call to action for Aboriginal and Torres Strait Islander leadership in the Australian mental health system. Advances in Mental Health 14:126–39.
-
Dudgeon P, Calma T & Holland C 2017. The context and causes of the suicide of Indigenous people in Australia. Journal of Indigenous Wellbeing 2:5–15.
-
Dudgeon P, Cox K, D'Anna D, Dunkley C, Hams K, Kelly K et al. 2012. Hear Our Voices: Community Consultations for the Development of an Empowerment, Healing and Leadership Program for Aboriginal people living in the Kimberley, Western Australia - Final Research Report. Perth: Telethon Institute for Child Health Research.
-
Dudgeon P, Milroy J, Calma T, Luxford Y, Ring IT, Walker R et al. 2016b. Solutions That Work: What the evidence and our people tell us. Perth: ATSISPEP.
-
Dudgeon P, Walker R, Scrine C, Shepherd CCJ, Calma T & Ring IT 2014. Effective strategies to strengthen the mental health and wellbeing of Aboriginal and Torres Strait Islander people. (ed., AIHW & AIFS). Canberra: Closing the Gap Clearinghouse.
-
Education and Health Standing Committee 2016. Learnings from the message stick: the report of the inquiry into Aboriginal youth suicide in remote areas. Perth: Education and Health Standing Committee.
-
Einsiedel LJ, van Iersel E, Macnamara R, Spelman T, Heffernan M, Bray L et al. 2013. Self-discharge by adult Aboriginal patients at Alice Springs Hospital, Central Australia: insights from a prospective cohort study. Australian Health Review 37:239–45.
-
FaHCSIA 2015. Footprints in Time: The Longitudinal Study of Indigenous Children Key Summary Report from Wave 5. Canberra: FaHCSIA.
-
Fairthorne J, Walker R, de Klerk N & Shepherd CCJ 2016. Early mortality from external causes in Aboriginal mothers: a retrospective cohort study. BMC Public Health 16:1.
-
Fogliani R 2019. Inquest into the deaths of: Thirteen children and young persons in the Kimberley Region, Western Australia. Perth: Coroner's Court of Western Australia.
-
Gee G, Dudgeon P, Schultz C, Hart A & Kelly K 2014. Aboriginal and Torres Strait Islander social and emotional wellbeing. In: Dudgeon P, Milroy H & Walker R (eds). Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice. Canberra: Commonwealth of Australia, 55–68.
-
Government of Western Australia 2020. McGowan Government releases commitment to Aboriginal youth wellbeing Media Statement.
-
Haswell MR, Blignault I, Fitzpatrick S & Jackson Pulver L 2013. The social and emotional wellbeing of Indigenous youth: Reviewing and extending the evidence and examining its implications for policy and practice. Sydney: Muru Marri, UNSW.
-
Hawthorne M 2018. Traditional Aboriginal healing and western medicine meet with Ngangkari project. Australian Medicine 30:9.
-
Jones R, Thurber K, Wright A, Chapman J, Donohoe P, Davis V et al. 2018. Associations between Participation in a Ranger Program and Health and Wellbeing Outcomes among Aboriginal and Torres Strait Islander People in Central Australia: A Proof of Concept Study. International journal of environmental research and public health 15:1478.
-
Jongen CS, McCalman J & Bainbridge RG 2019. A systematic scoping review of school-based resilience interventions for Indigenous adolescents in CANZUS nations. Frontiers in public health 7:351.
-
Just Reinvest NSW Inc. Justice Reinvestment in Bourke. Viewed 21 October 2020.
-
Kahneman D & Deaton A 2010. High income improves evaluation of life but not emotional well-being. Proceedings of the National Academy of Sciences 107:489–93.
-
Kelaher MA, Ferdinand AS & Paradies Y 2014. Experiencing racism in health care: The mental health impacts for Victorian Aboriginal communities. The Medical Journal of Australia 201:44–7.
-
KPMG Australia & Just Reinvest NSW Inc. 2018. Maranguka Justice Reinvestment Project: Impact Assessment. NSW: Just Reinvest NSW.
-
Laverty M, McDermott DR & Calma T 2017. Embedding cultural safety in Australia’s main health care standards. The Medical Journal of Australia 207:15–6.
-
Leckning B, Borschmann R, Guthridge S, Bradley P, Silburn S & Robinson G 2020. Aboriginal and non-Aboriginal emergency department presentations involving suicide-related thoughts and behaviors. Crisis : the journal of crisis intervention and suicide prevention 41:459–68.
-
Leckning B, Ringbauer A, Robinson G, Carey T, Hirvonen T & Armstrong G 2019. Guidelines for best practice psychosocial assessment of Aboriginal and Torres Strait Islander people presenting to hospital with self-harm and suicidal thoughts. Darwin: Menzies School of Health Research.
-
Macedo D, Smithers LG, Roberts RM, Paradies Y & Jamieson L 2019a. Effects of racism on the socio-emotional wellbeing of Aboriginal Australian children. International Journal for Equity in Health 18:132.
-
Macedo DM, Smithers LG, Roberts RM, Haag DG, Paradies Y & Jamieson LM 2019b. Does ethnic-racial identity modify the effects of racism on the social and emotional wellbeing of Aboriginal Australian children? PloS one 14:e0220744.
-
MacLean S, Ritte R, Thorpe A, Ewen S & Arabena K 2017. Health and wellbeing outcomes of programs for Indigenous Australians that include strategies to enable the expression of cultural identities: a systematic review. Australian journal of primary health 23:309–18.
-
Manning M, Ambrey C & Fleming C 2016. A Longitudinal Study of Indigenous Wellbeing in Australia. Journal of Happiness Studies 17:2503–25.
-
Mia T, Dudgeon P, Mascall C, Grogan G, Murray B & Walker R 2017. An evaluation of the national empowerment project cultural, social, and emotional wellbeing program. Journal of Indigenous Wellbeing 2:33-48.
-
National Coronial Information System 2020. NCIS fact sheet: Intentional self-harm deaths of young persons in Australia. Melbourne: NCIS.
-
NIAA (National Indigenous Australians Agency) 2019. Summary of Evaluation of Mental Health First Aid Training on Groote Eylandt and Bickerton Island. Australia.
-
Ou L, Chen J, Hillman K & Eastwood J 2010. The comparison of health status and health services utilisation between Indigenous and non-Indigenous infants in Australia. Australian & New Zealand Journal of Public Health 34:50–6.
-
Paradies YC & Cunningham J 2012. The DRUID study: racism and self-assessed health status in an Indigenous population. BMC Public Health 12:131.
-
Parker R & Milroy H 2014. Aboriginal and Torres Strait Islander Mental Health: An Overview. In: Dudgeon P, Milroy H & Walker R (eds). Working Together: Aboriginal and Torres Strait Islander Mental Health and Wellbeing Principles and Practice. Canberra: Commonwealth of Australia, 25–38.
-
PM&C (Department of the Prime Minister and Cabinet) 2019. Stories from Country 2015-2017: How Indigenous Rangers and Indigenous Protected Areas are strengthening connections to country, culture and community. Canberra: PM&C.
-
QMHC (Queensland Mental Health Commission) 2020. Don't Judge, and Listen: Experiences of stigma and discrimination related to problematic alcohol and other drug use. Brisbane: Queensland Mental Health Commission.
-
Ridani R, Shand FL, Christensen H, McKay K, Tighe J, Burns J et al. 2015. Suicide Prevention in Australian Aboriginal Communities: A Review of Past and Present Programs. Suicide and Life-Threatening Behavior 45:111–40.
-
Salmon M, Skelton F, Thurber K, Bennetts Kneebone L, J G, Lovett R et al. 2018. Intergenerational and early life influences on the well-being of Australian Aboriginal and Torres Strait Islander children: overview and selected findings from Footprints in Time, the Longitudinal Study of Indigenous Children. . Journal of Developmental Origins of Health and Disease:1–7.
-
Shadforth G & Shadforth S 2018. YEaHCC (Youth Empowerment and Healing Cultural Camp): A youth suicide prevention initiative at a grassroots level to lead real action and mobilise change amongst those who are continuously being affected by the impacts of suicide across the Kimberley region. Perth, Australia.
-
Skerrett DM, Gibson M, Darwin L, Lewis S, Rallah R & De Leo D 2018. Closing the gap in Aboriginal and Torres Strait Islander youth suicide: A social–emotional wellbeing service innovation project. Australian Psychologist 53:13–22.
-
Social Health Reference Group 2004. National Strategic Framework for Aboriginal and Torres Strait Islander Peoples' Mental Health and Social and Emotional Well Being (2004-2009). Canberra: Aboriginal Health & Medical Research Council of NSW.
-
Strazdins L, Shipley M, Clements M, Obrien LV & Broom DH 2010. Job quality and inequality: parents' jobs and children's emotional and behavioural difficulties. Social Science & Medicine 70:2052–60.
-
The Centre for Best Practice in Aboriginal and Torres Strait Islander Suicide Prevention 2022. Healing and Social and Emotional Wellbeing. CBPATSISP. Viewed November 2022.
-
The Healing Foundation. Stolen Generations Projects. Viewed 12 October 2020.
-
The National Empowerment Project 2019. Cultural, Social and Emotional Wellbeing Program Evaluation, Perth 2018–2019. Transforming Indigenous Mental Health and Wellbeing.
-
Thurber K, Walker J, Walter M, Dunbar T, Guthrie J, Batteram P et al. 2019. Technical report: Measuring adult mental health, psychological distress, and social and emotional wellbeing in the longitudinal study of Indigenous children. Canberra: Aboriginal and Torres Strait Islander Health Program at the National Centre for Epidemiology and Population Health, Research School of Population health, Australian National University.
-
Tighe J & McKay K 2012. Alive and Kicking Goals!: Preliminary findings from a Kimberley suicide prevention program. Advances in Mental Health 10:240–5.
-
Twizeyemariya A, Guy S, Furber G & Segal L 2017. Risks for mental illness in Indigenous Australian children: a descriptive study demonstrating high levels of vulnerability. The Milbank Quarterly 95:319–57.
-
Victorian Government, New South Wales Government & Australian Government 2020. National Mental Health and Wellbeing Pandemic Response Plan. Victorian Government, New South Wales Government and Australian Government.
-
WHO 2020. Social determinants of health. Geneva: WHO. Viewed 8 October 2020.
-
Yashadhana A, Pollard-Wharton N, Zwi A & Biles B 2020. Indigenous Australians at increased risk of COVID-19 due to existing health and socioeconomic inequities. The Lancet Regional Health - Western Pacific 1.
-
Young C, Craig JC, Clapham K, Banks S & Williamson A 2019. The prevalence and protective factors for resilience in adolescent Aboriginal Australians living in urban areas: a cross‐sectional study. Australian and New Zealand journal of Public Health 43:8–14.

