Key messages
- Respiratory diseases were the fourth leading cause of death for Aboriginal and Torres Strait Islander people. In the period 2015–2019, there were 1,498 deaths (10% of all deaths) of Indigenous Australians due to respiratory diseases.
- Rates of death due to specific respiratory diseases were similar for Indigenous males and females. The major contributor was chronic obstructive pulmonary disease (937 deaths or 63% of all deaths due to respiratory diseases). It was followed by pneumonia and influenza (247 deaths or 17%).
- Over the decade 2010 to 2019, there was a 22% increase in the age-standardised death rate due to respiratory diseases for Indigenous Australians and the gap in the rates for Indigenous and non-Indigenous Australians widened by 43%.
- Between July 2017 and June 2019, there were 59,301 hospitalisations due to respiratory disease among Indigenous Australians (5.4% of total Indigenous hospitalisations).
- Over the same period, 20% of respiratory disease hospitalisations were due to pneumonia, with a further 20% due to bronchitis and emphysema (also 20%).
- The hospitalisation rate for respiratory diseases for Indigenous Australians was highest for those aged 65 and over (110 per 1,000), followed by those aged 0–4 (85 per 1,000).
- Indigenous Australians living in Remote areas were 2.4 times as likely to be hospitalised for respiratory diseases compared with those living in Major cities (65 and 27 per 1,000, respectively).
- Over the decade 2009–10 to 2018–19, there was a 32% increase in the age-standardised hospitalisation rate for Indigenous Australians due to respiratory diseases.
Why is it important?
Respiratory diseases, such as asthma, chronic obstructive pulmonary disease (COPD) (including chronic bronchitis and emphysema), pneumonia and invasive pneumococcal disease, are a major cause of poor health and death for Aboriginal and Torres Strait Islander people. Almost half (47%) of the respiratory disease burden among Indigenous Australians in 2018 was attributed to smoking (AIHW 2022).
High rates of pneumonia are associated with factors such as other respiratory diseases, poor living conditions, malnutrition, smoking and harmful use of alcohol (Grau et al. 2014; Janu et al. 2014; Lim et al. 2014). Pneumococcal immunisation programs targeting Indigenous Australians demonstrate substantially lower coverage than recommended (NACCHO & RACGP 2018). Young children and those in older age groups are most at risk. Indigenous children in the Northern Territory have a rate of radiologically confirmed pneumonia (that is, determined by a chest x-ray) that is among the highest in the world (O’Grady et al. 2010).
Asthma can affect physical functioning and attendance at school and work. It commonly coexists with other chronic conditions and low socioeconomic status. Deaths due to asthma occur in all age groups, but the risk of dying from asthma increases with age.
COPD is a serious lung disease that mainly affects older people and is associated with and caused by smoking, environmental pollutants and childhood infectious diseases such as pneumonia and bronchitis (AIHW 2019). Currently, 41% of Indigenous Australians aged 15 and over smoke, 2.9 times the non-Indigenous rate (see measure 2.15 Tobacco use). COPD is characterised by chronic obstruction of lung airflow that interferes with breathing. An analysis has found that among Indigenous Australians aged 55 and over that were hospitalised for COPD, cancer is a common comorbidity (AIHW 2011). The impaired lung function of people with COPD increases their lung cancer risk, and the risk of lung cancer is much higher in COPD patients with severe disease (AIHW 2014).
Burden of disease
In 2018, respiratory diseases caused an estimated 17,920 years of healthy life lost due to illness and or death (17,920 Disability-Adjusted Life Years or DALY) (excludes acute infections such as influenza) – accounting for 7.5% of the total burden of disease for Indigenous Australians.
Respiratory diseases accounted for 9% of the total non-fatal burden (years lived in ill health or with disability (YLD)) for Indigenous Australians and 5.8% of the fatal burden (premature death (YLL)).
Of the total burden due to respiratory diseases, a larger proportion was experienced by Indigenous females (54%) than Indigenous males (46%). Asthma was the leading cause of respiratory burden among Indigenous Australians under 45 years (80% of total respiratory burden for this age group), while COPD was the leading cause of respiratory burden for those aged 45 and older (65% of total respiratory burden for this age group) (AIHW 2022).
The age-standardised burden due to respiratory diseases for Indigenous Australians was 2.7 times the rate for non-Indigenous Australians (AIHW 2022).
Between 2003 and 2018, the age-standardised rate of total burden due to respiratory diseases for Indigenous Australians decreased slightly (from 38 to 34 DALY per 1,000 people). This was driven by a decrease in the fatal burden, mainly from COPD. The rate of non-fatal burden due to respiratory diseases remained relatively stable (20 and 19 YLD per 1,000, respectively) (AIHW 2022).
Data findings
Deaths from respiratory diseases
Mortality data in this measure are from five jurisdictions for which the quality of Indigenous identification in the deaths data is considered to be adequate: namely, New South Wales, Queensland, Western Australia, South Australia and the Northern Territory. Data by remoteness are reported for all Australian states and territories combined (see Data sources: National Mortality Database).
In the period 2015–2019, there were 1,498 deaths of Indigenous Australians due to respiratory diseases, corresponding to 42 deaths per 100,000 population. Respiratory diseases were the fourth leading cause of death for Indigenous Australians, responsible for 10% of deaths (Table D1.23.1). After adjusting for differences in the age structure between the two populations, the death rate due to respiratory diseases for Indigenous Australians was twice the rate for non-Indigenous Australians.
For Indigenous Australians, the death rate due to respiratory diseases was highest in the Northern Territory (62 per 100,000) followed by Western Australia (43 per 100,000), New South Wales (41 per 100,000), South Australia (38 per 100,000) and Queensland (36 per 100,000) (Table D1.23.2, Figure 1.04.1). Though not the highest population rate, New South Wales accounted for the highest proportion of respiratory deaths, reflecting that it has the largest Indigenous population – over one-third (37%) of all deaths due to respiratory diseases in the five jurisdictions combined. Respiratory diseases were also responsible for a higher proportion of total deaths within New South Wales (12%) than in the other four jurisdictions (8–9%) (Table D1.23.2).
Figure 1.04.1: Death rates due to respiratory diseases among Indigenous Australians, by state and territory, NSW, Qld, WA, SA and NT, 2015–2019
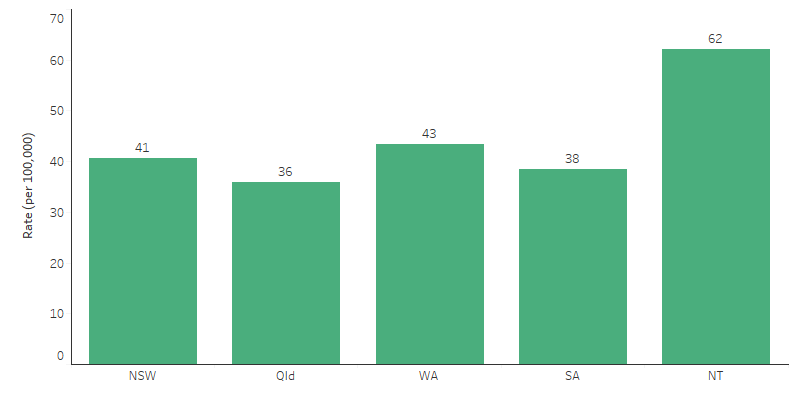
Source: Table D1.23.2. AIHW National Mortality Database.
Of all respiratory diseases deaths among Indigenous Australians in 2015–2019:
- 63% (937) were due to COPD,
- 17% (247) were due to pneumonia and influenza, and
- 5% (74) were due to asthma.
Rates of death due to specific respiratory diseases were similar for Indigenous males and females (Figure 1.04.2). The only statistically significant difference in rates by sex was for asthma, where the rate for females was slightly higher than that of males (2.6 compared with 1.6 per 100,000 population).
After adjusting for differences in the age structure between the two populations, the rate of deaths due to COPD for Indigenous Australians was 2.8 times that of non-Indigenous Australians. Rates of deaths due to asthma; and pneumonia and influenza were also higher for Indigenous Australians than non-Indigenous Australians (rate ratios of 2.5 and 1.3, respectively) (Table D1.23.14).
Figure 1.04.2: Mortality rates due to respiratory diseases for Indigenous Australians, by sex, NSW, Qld, WA, SA and NT, 2015–2019
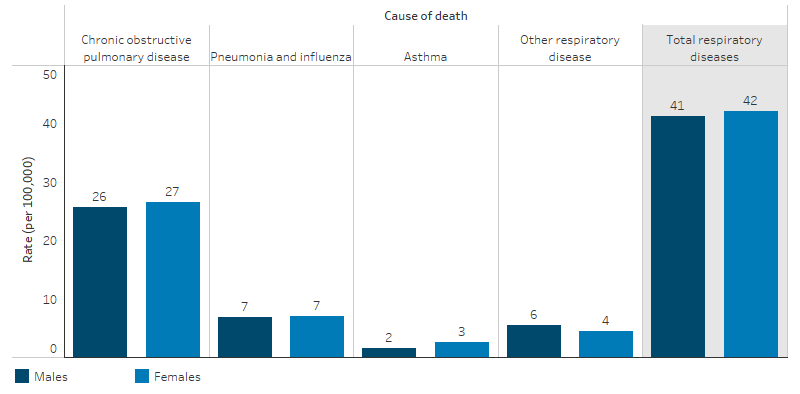
Source: Table D1.23.14. AIHW National Mortality Database.
For Indigenous Australians the leading causes of death due to respiratory diseases varied by age. For those aged between 0–14 and 35–44 the leading cause of respiratory death was due to pneumonia and influenza (72% and 40% of respiratory deaths respectively). For those aged 25–34 the leading cause was asthma (31%) and for those aged 45 and older the leading cause was COPD (between 59%–74%) (Table D1.23.15).
In the 2015–2019 period, for Indigenous Australians the proportion of total deaths due to respiratory diseases were similar in non-remote and remote areas (10% for Major cities, Inner and Outer regional areas, compared to 9% in Remote and very remote areas). However, for Indigenous Australians the rate of deaths due to respiratory disease in remote areas was 1.6 times as high as that in non-remote areas (57 compared with 36 per 100,000, respectively).
In remote areas, the death rate from respiratory diseases for Indigenous Australians was 2.8 times that of non-Indigenous Australians, while in non-remote areas, the rate for Indigenous Australians was 1.8 times that of non-Indigenous Australians (based on age-standardised rates, Table D1.23.30).
Prevalence from the ABS survey
Reported data on respiratory diseases is available from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey. Based on these data, in 2018–19, an estimated 29% of Indigenous Australians (238,020) had a respiratory disease lasting or likely to last 6 months or more (Table D1.04.2). After adjusting for differences in the age structure between the two populations, the proportion of Indigenous and non-Indigenous Australians reporting respiratory disease was similar (Table D1.04.3).
The most commonly reported respiratory conditions for Indigenous Australians were asthma (16%), chronic sinusitis (7.4%) and COPD (3.4%). After adjusting for differences in the age structure between the two populations, Indigenous Australians were 2.2 times as likely to report COPD (5% and 2%, respectively) and 1.6 times as likely to report asthma as non‑Indigenous Australians (18% and 11%, respectively) (Figure 1.04.3) (ABS 2019).
Figure 1.04.3: Age-standardised proportion reporting respiratory disease, by Indigenous status, 2018–19
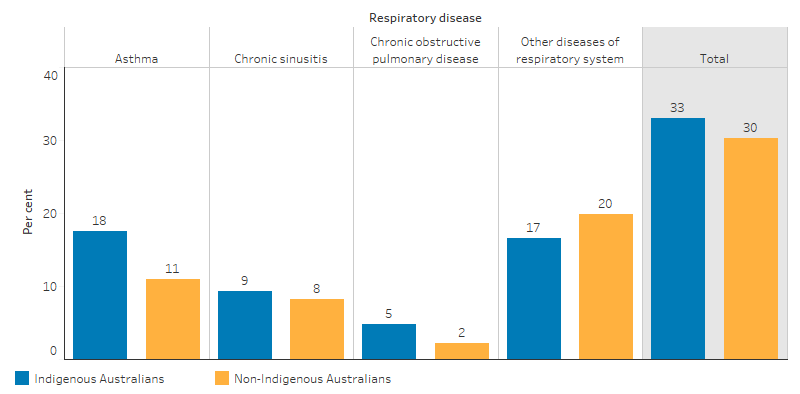
Source: National Aboriginal and Torres Strait Islander Health Survey 2018–19 (ABS Table 6.3).
In 2018–19, Indigenous females (32%) reported a higher rate of respiratory diseases compared with Indigenous males (26%).
There was also an increase in the rate of respiratory diseases as age increased, ranging from 19% for Indigenous Australians aged 0–14, to 37% in the 45–54 age group (Table D1.04.2).
Indigenous Australians living in non-remote areas (32%) reported a higher rate of respiratory disease than those in remote areas (15%). By jurisdiction, Indigenous Australians living in Tasmania reported the highest rate (43%), while those in the Northern Territory reported the lowest (12%).
Looking specifically at asthma, the proportion of reported asthma for Indigenous Australians was 16% in 2018–19, about the same as in 2012–13 (18%) (10). Indigenous females (18%) reported a higher rate of asthma compared with Indigenous males (13%). Indigenous Australians living in remote areas (9%) were less likely to report asthma than those in non-remote areas (17%).
By jurisdiction, in 2018–19, the highest rates of asthma were reported by Indigenous Australians in the Australian Capital Territory (25%) and South Australia (23%), with the lowest in the Northern Territory (6%). By age, asthma prevalence was higher in older age groups, ranging from 12% for ages 0–14, to 26% for ages 55+.
In 2018–19, of Indigenous Australians who still get asthma or have had symptoms in the last 12 months, one-third (32%) had a written asthma action plan. Three in ten (30%) indicated that their asthma got worse or out of control in the last 12 months, but half of these (15%) reported they did not go to the hospital when this happened. Of those with asthma or symptoms in the last 12 months, just over half (56%) reported using asthma medication within the last 2 weeks (D1.04.20).
Hospitalisations
Hospitalisation statistics are a measure of the occurrence of conditions requiring acute care. It is important to note that levels of hospital use do not necessarily reflect prevalence or incidence of diseases in the community.
Between July 2017 and June 2019, there were 59,301 hospitalisations (a rate of 36 per 1,000 population) with a principal diagnosis of respiratory disease among Indigenous Australians (5.4% of total Indigenous hospitalisations, excluding dialysis) (Table D1.02.5).
The hospitalisation rate for respiratory diseases for Indigenous Australians was highest for those aged 65 and over (110 hospitalisations per 1,000 population), followed by those aged 0–4 (85 per 1,000) (Table D1.04.8, Figure 1.04.4).
Figure 1.04.4: Age-specific hospitalisation rates for diseases of the respiratory system (based on principal diagnosis), by Indigenous status and age, Australia, July 2017 to June 2019
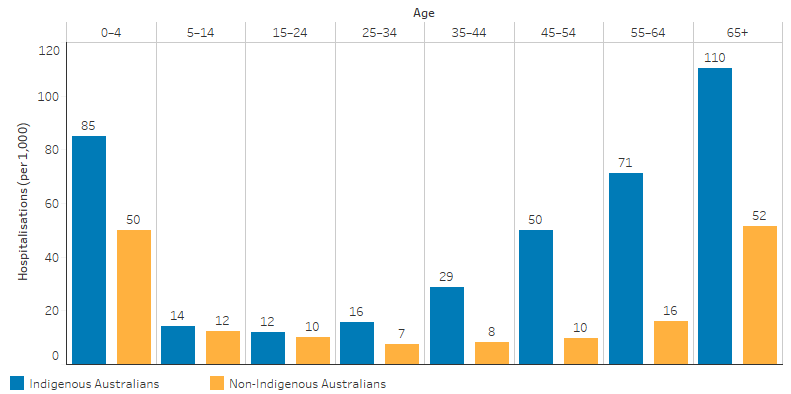
Source: Table D1.04.8. AIHW analysis of National Hospital Morbidity Database.
Across all age groups, the hospitalisation rate for respiratory diseases was higher for Indigenous Australians than for non-Indigenous Australians (Table D1.04.8, Figure 1.04.4). The largest relative difference was among those aged 45–54, where the rate for Indigenous Australians was 5.1 times the rate for non-Indigenous Australians.
After adjusting for differences in the age structure between the two populations, the hospitalisation rate of Indigenous Australians for respiratory diseases was 2.4 times the rate for non‑Indigenous Australians (Table D1.04.7).
In the period from July 2017 to June 2019, pneumonia accounted for 20% of respiratory disease hospitalisations, with bronchitis and emphysema combined accounting for a further 20% (Table D1.04.10).
The greatest differences in hospitalisation rates for respiratory disease between Indigenous and non-Indigenous Australians were for bronchitis and emphysema combined (a difference of 10.5 per 1,000) and pneumonia (a difference of 7.2 per 1,000) (Table D1.04.10).
Indigenous Australians aged 35–44 were 18 times as likely as non-Indigenous Australians to be hospitalised for bronchitis and emphysema (Table D1.04.16).
Looking at data by state and territory, the hospitalisation rate of Indigenous Australians for respiratory diseases was highest in the Northern Territory (63 hospitalisations per 1,000 population) followed by Western Australia (43 per 1,000) (Table D1.04.7, Figure 1.04.5).
Figure 1.04.5: Hospitalisation rates among Indigenous Australians for diseases of the respiratory system (based on principal diagnosis), by jurisdiction, Australia, July 2017 to June 2019
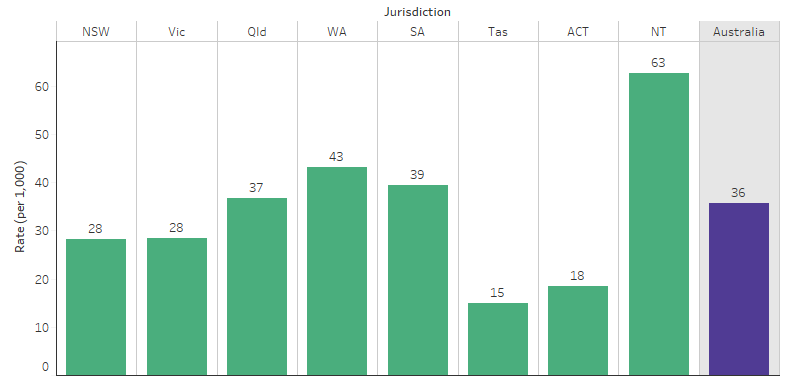
Source: Table D1.04.7. AIHW analysis of National Hospital Morbidity Database.
Across remoteness areas, Indigenous Australians living in Remote and Very remote areas had a higher rate of hospitalisation due to respiratory diseases (65 and 58 hospitalisations per 1,000 population, respectively), than those living in non-remote areas (between 27 and 38 per 1,000, depending on area). In contrast, the rate was similar across remoteness areas for non-Indigenous Australians.
Between July 2017 and June 2019, Indigenous Australians living in Remote areas were 2.4 times as likely to be hospitalised for respiratory diseases as those living in Major cities (65 and 27 per 1,000, respectively) (Table D1.04.9, Figure 1.04.6).
Figure 1.04.6: Hospitalisations among Indigenous Australians for diseases of the respiratory system (based on principal diagnosis), by remoteness, Australia, July 2017 to June 2019
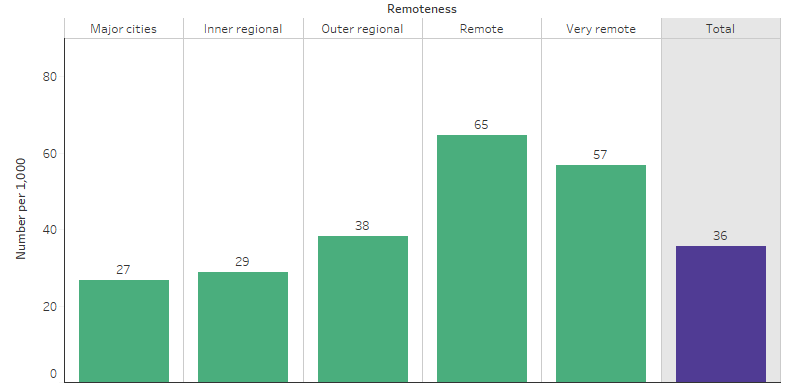
Source: Table D1.04.9. AIHW analysis of National Hospital Morbidity Database.
Considering hospitalisations for respiratory diseases by jurisdiction and remoteness, the largest relative difference between Indigenous and non-Indigenous Australians was in remote areas (Remote and Very remote areas combined) of Western Australia, followed by remote areas of South Australia (where the rates for Indigenous Australians were 4.9 times and 4.1 times the rates for non-Indigenous Australians, respectively) (Table D1.04.17).
Notifiable diseases
Notifiable diseases data are collected by States and Territories under their public health legislation. This legislation has required medical practitioners, and some other classes of people, to notify health authorities of certain communicable and other diseases (Department of Health 2003).
Infection with invasive Streptococcus pneumoniae is responsible for significant morbidity and mortality worldwide, especially in the very young, the elderly and those with predisposing risk factors (Department of Health 2016). In the three-year period of 2016–2018 there were 626 notifications of invasive pneumococcal disease for Indigenous Australians, representing 14% of all cases notified (Table D1.04.15).
Change over time in deaths and hospitalisations
Between 2006 and 2019 there was no significant change in the age-standardised death rate due to respiratory diseases for Indigenous Australians, nor in the gap between Indigenous and non-Indigenous Australians. Over the decade 2010 to 2019, there was a 22% increase in the age-standardised death rate due to respiratory diseases for Indigenous Australians and the gap in the rates for Indigenous and non-Indigenous Australians widened by 43% (Table D1.23.21).
Between 2009–10 and 2018–19, after adjusting for changes in the population over time, there was a 32% increase in the hospitalisation rate for Indigenous Australians due to respiratory diseases in the six jurisdictions combined with Indigenous identification data of adequate quality (New South Wales, Victoria, Queensland, Western Australia, South Australia and the Northern Territory) (Table D1.04.11, Figure 1.04.7).
Figure 1.04.7: Age-standardised hospitalisation rates for diseases of the respiratory system (based on principal diagnosis), by Indigenous status, NSW, Vic, Qld, WA, SA and NT, 2006–07 to 2018–19
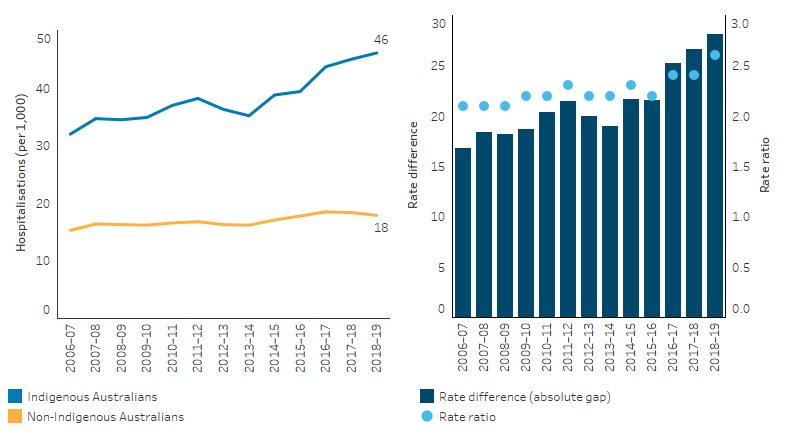
Note: Rate difference is the age-standardised rate (per 1,000) for Indigenous Australians minus the age-standardised rate (per 1,000) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D1.04.11. AIHW analysis of National Hospital Morbidity Database.
Based on age-standardised rates, hospitalisation due to respiratory diseases increased faster for Indigenous Australians compared with non-Indigenous Australians, resulting in a widening of the gap (increasing from 19 per 1,000 in 2009–10 to 28 per 1,000 in 2018–19) (Table D1.04.11).
The hospitalisation rate due to respiratory diseases for Indigenous children aged 0–4 increased by 35% in the same six jurisdictions combined over the same period (Table D1.04.12).
Research and evaluation findings
A recent study in the Northern Territory found that Indigenous patients referred to respiratory specialist outreach teams in remote and rural communities have a significantly higher rate of smoking and COPD compared with non-Indigenous patients referred to this service. Bronchiectasis is also more common among Indigenous patients (Kruavit et al. 2017). The study suggested there is a need to focus resources on reducing the rate of smoking in these areas, and further improve the quality of health care with a focus on primary health care. In addition to education provided by the respiratory outreach team, Indigenous health workers could provide information on tobacco and quit support to the community. Another recent study conducted in the Top End found that Indigenous patients with COPD had a higher prevalence of smoking, moderate to severe airflow obstruction on spirometry and were frequently co-diagnosed with bronchiectasis with increased severity of ventilatory impairment, compared with Indigenous patients who did not have a diagnosis of COPD (Heraganahally et al. 2019).
Research conducted in the United States suggested that public health approaches, such as tobacco control, addressing air pollution and occupational exposures, have the best chance of substantially reducing the burden of lung disease around the world. These could have enormous effects on reducing morbidity and mortality caused by lung disease (Schluger & Koppaka 2014). The World Health Organization Framework Convention on Tobacco Control acknowledges the need to take measures to promote the participation of indigenous peoples and communities in the development, implementation and evaluation of tobacco control programs (WHO 2003). It recognises the effectiveness and importance of non-price measures in reducing the demand for tobacco, including protection from exposure to tobacco smoke, and education, communication, training and public awareness.
A recent overview of respiratory diseases in Indigenous children found a lack of research among Indigenous children living in urban and regional areas, as most research has been conducted in remote areas (Australian Indigenous HealthInfoNet 2020). The overview identified a 2013–2015 study of Indigenous children who visited the Caboolture Community Medical clinic in northern Brisbane, which found that 33% had symptoms of an acute respiratory infection, and 22% went to the clinic specifically because of an acute respiratory infection (Hall et al. 2017). A subsequent study of mostly Indigenous children who visited the Caboolture Community Medical clinic over a similar period in 2013–2015 found that, in an average month, about one-quarter of the children were attending the clinic with an acute respiratory infection with a cough. The study results indicated that one in five children will develop a chronic cough following acute respiratory infections with a cough. The overview also identified several community-based studies in remote areas. A 2010–2013 study of Indigenous children from 25 remote communities in the Northern Territory found that 59% of children had a runny nose and 39% had a cough (Leach et al. 2016). Another study of Indigenous children born between 2001 and 2006 in five remote communities in the Northern Territory found that by the time they turned one year old, 96% of babies had gone to their health service with at least one infection, many infections were recurrent, and infections of the upper respiratory tract were the most common (Kearns et al. 2013).
Universal pneumococcal conjugate vaccine (PCV) programs began for Indigenous Australian children in 2001 and all Australian children in 2005, and 13-valent PCV was introduced in 2011 (Meder et al. 2020). To help prevent pneumococcal disease it is recommended that Indigenous children are vaccinated with 13-valent PCV at 2, 4 and 6 months of age, with an additional dose given at 12–18 months of age if living in Queensland, the Northern Territory, Western Australia or South Australia (NACCHO & RACGP 2018). An assessment of the effect of PCV examined acute lower respiratory infection (ALRI) hospitalisations of Indigenous infants in the Northern Territory from 2006 to 2015, across three periods of different PCV use (Binks et al. 2020). The study found that there was a 30% reduction in bacterial-coded pneumonia hospitalisations during the 2011–2015 period in which 13-valent PCV was used. The authors concluded that while the findings supported the use of this vaccine, one in five Indigenous infants continued to be hospitalised with an ALRI within their first year of life, and a combination of environmental and biomedical approaches are needed.
Researchers have conducted a range of studies of respiratory disease services. These include a study in Western Australia that found that the implementation of an integrated COPD multidisciplinary community service reduced respiratory hospitalisations in the long term (Chung et al. 2016). A large pilot study in Queensland showed the importance of working with communities and Indigenous staff in the development and delivery of a culturally appropriate and accessible specialist respiratory service (Medlin et al. 2014). The Indigenous Respiratory Outreach Care (IROC) program aims to develop and deliver culturally appropriate specialist respiratory outreach services and resources to Indigenous Australians in rural and remote Queensland communities, improve access to specialist respiratory services; and increase awareness of lung health in Indigenous communities. A study of children attending IROC clinics found that the model of care led to significant lung function improvement for Indigenous children with asthma and bronchiectasis (Collaro et al. 2020). Researchers in New Zealand also found that Māori participants felt strongly discouraged to attend pulmonary rehabilitation when culturally appropriate communication and relationship-building was absent (Levack et al. 2016).
Indigenous Australians experience a range of pre-existing health risks and social disadvantage that increase the risk of severe illness or death if infected with COVID-19 when compared to non-Indigenous Australians. Indigenous Australians have higher prevalence of chronic conditions, such as respiratory diseases, diabetes, and cardiovascular diseases, which are known to increase the risk of severe illness and death from COVID-19. The COVID-19 pandemic has highlighted the need for swift action to ensure implementation of equitable and appropriate prevention, treatment, and management measures to vulnerable population groups (Yashadhana et al. 2020).
Implications
Over the decade 2010 to 2019 there has been a significant increase in respiratory disease death rates for Indigenous Australians and a widening of the gap with non-Indigenous Australians. Further, self-reported respiratory diseases, hospitalisation and death rates are still around twice as high for Indigenous Australians compared with non-Indigenous Australians. While rates of reported asthma and COPD for Indigenous Australians were similar in 2012–13 and 2018–19 (ABS 2019), overall, there was a 32% increase in the age-standardised hospitalisation rate for Indigenous Australians due to respiratory diseases between 2009–10 and 2018–19. Chronic respiratory diseases, especially COPD and asthma, are major contributors to the burden of disease for Indigenous Australians.
While it is important to manage patients with chronic respiratory diseases effectively, much of this burden is preventable and public health approaches are critical to prevent their occurrence. Initiatives addressing smoking (including second-hand smoke), immunisation, living conditions, overcrowded housing, chronic disease and access to health care are likely to contribute to improvements in respiratory disease (Johnston et al. 2010; Torzillo & Chang 2014). Culturally appropriate communication and health services are essential to ensure Indigenous Australians feel comfortable to participate in disease prevention and medical therapies.
Further research into individual respiratory conditions for Indigenous Australians is needed particularly in non-remote settings. The aggregated statistics provide an unclear picture, with higher self-reported prevalence in non-remote areas, but higher hospitalisations in remote areas. The degree to which this reflects issues around access to health care and the severity of particular acute illnesses requiring hospitalisation in remote areas, or the validity of the self-report survey data in remote areas, is not clear. Nationally, a number of health policies have been implemented to reduce the burden of chronic respiratory disease among Indigenous Australians, including the Tackling Indigenous Smoking program and Indigenous specific chronic disease support activities under the Indigenous Australians’ Health Programme, National Strategic Action Plan for Lung Conditions and the National Asthma Strategy.
The data in this measure predate the arrival of COVID-19. An analysis of the impact of COVID-19 on Indigenous Australians will be a topic for future research.
The policy context is at Policies and strategies.
References
- ABS (Australian Bureau of Statistics) 2019. National Aboriginal and Torres Strait Islander Health Survey, 2018–19. 4715.0. Canberra: ABS.
- AIHW (Australian Institute of Health and Welfare) 2011. Asthma in Australia 2011: with a focus chapter on chronic obstructive pulmonary disease. Canberra: AIHW.
- AIHW 2014. Coronary heart disease and chronic obstructive pulmonary disease in Indigenous Australians. Canberra: AIHW.
- AIHW 2019. Chronic obstructive pulmonary disease (COPD). Canberra: AIHW.
- AIHW 2022. Australian Burden of Disease Study: Impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2018. Canberra: AIHW.
- Australian Indigenous HealthInfoNet 2020. Summary of respiratory diseases among Aboriginal and Torres Strait Islander children. Perth, WA.
- Binks MJ, Beissbarth J, Oguoma VM, Pizzutto SJ, Leach AJ, Smith-Vaughan HC et al. 2020. Acute lower respiratory infections in Indigenous infants in Australia's Northern Territory across three eras of pneumococcal conjugate vaccine use (2006–15): a population-based cohort study. The Lancet Child & Adolescent Health 4:425-34.
- Chung LP, Lake F, Hyde E, McCamley C, Phuangmalai N, Lim M et al. 2016. Integrated multidisciplinary community service for chronic obstructive pulmonary disease reduces hospitalisations. Internal Medicine Journal 46:427-34.
- Collaro AJ, Chang AB, Marchant JM, Masters IB, Rodwell LT, Takken AJ et al. 2020. Culturally Appropriate Outreach Specialist Respiratory Medical Care Improves the Lung Function of Children in Regional and Remote Queensland. Lung:1-9.
- Department of Health (Australian Government Department of Health) 2003. Notifiable diseases surveillance, 1917 to 1991. Canberra: Department of Health. Viewed 25/09/2020.
- Department of Health 2016. Pneumococcal disease: Invasive pneumococcal disease in Australia annual reports. Canberra: Department of Health. Viewed 25/09/2020.
- Grau I, Ardanuy C, Calatayud L, Schulze MH, Linares J & Pallares R 2014. Smoking and alcohol abuse are the most preventable risk factors for invasive pneumonia and other pneumococcal infections. International Journal of Infectious Diseases 25:59-64.
- Hall KK, Chang AB, Anderson J, Dunbar M, Arnold D & O'Grady KAF 2017. Characteristics and respiratory risk profile of children aged less than 5 years presenting to an urban, Aboriginal‐friendly, comprehensive primary health practice in Australia. Journal of paediatrics and child health 53:636-43.
- Heraganahally SS, Wasgewatta SL, McNamara K, Eisemberg CC, Budd RC, Mehra S et al. 2019. Chronic Obstructive Pulmonary Disease In Aboriginal Patients Of The Northern Territory Of Australia: A Landscape Perspective. International Journal of Chronic Obstructive Pulmonary Disease 14:2205.
- Janu EK, Annabattula BI, Kumariah S, Zajaczkowska M, Whitehall JS, Edwards MJ et al. 2014. Paediatric hospitalisations for lower respiratory tract infections in Mount Isa. The Medical Journal of Australia 200:591-4.
- Johnston V, Walker N, Thomas DP, Glover M, Chang AB, Bullen C et al. 2010. The study protocol for a randomized controlled trial of a family-centred tobacco control program about environmental tobacco smoke (ETS) to reduce respiratory illness in Indigenous infants. BMC Public Health 10:114.
- Kearns T, Clucas D, Connors C, Currie BJ, Carapetis JR & Andrews RM 2013. Clinic attendances during the first 12 months of life for Aboriginal children in five remote communities of northern Australia. PloS one 8:e58231.
- Kruavit A, Fox M, Pearson R & Heraganahally S 2017. Chronic respiratory disease in the regional and remote population of the Northern Territory Top End: A perspective from the specialist respiratory outreach service. Australian Journal of Rural Health 25:275-84.
- Leach A, Wigger C, Beissbarth J, Woltring D, Andrews R, Chatfield M et al. 2016. General health, otitis media, nasopharyngeal carriage and middle ear microbiology in Northern Territory Aboriginal children vaccinated during consecutive periods of 10-valent or 13-valent pneumococcal conjugate vaccines. International Journal of Pediatric Otorhinolaryngology 86:224-32.
- Levack WM, Jones B, Grainger R, Boland P, Brown M & Ingham TR 2016. Whakawhanaungatanga: the importance of culturally meaningful connections to improve uptake of pulmonary rehabilitation by Māori with COPD–a qualitative study. International Journal of Chronic Obstructive Pulmonary Disease 11:489.
- Lim FJ, Lehmann D, McLoughlin A, Harrison C, Willis J, Giele C et al. 2014. Risk factors and comorbidities for invasive pneumococcal disease in Western Australian Aboriginal and non-Aboriginal people. Pneumonia 4:24-34.
- Meder KN, Jayasinghe S, Beard F, Dey A, Kirk M, Cook H et al. 2020. Long-term Impact of Pneumococcal Conjugate Vaccines on Invasive Disease and Pneumonia Hospitalizations in Indigenous and Non-Indigenous Australians. Clinical Infectious Diseases 70:2607-15.
- Medlin LG, Chang AB, Fong K, Jackson R, Bishop P, Dent A et al. 2014. Indigenous Respiratory Outreach Care: the first 18 months of a specialist respiratory outreach service to rural and remote Indigenous communities in Queensland, Australia. Australian Health Review 38:447-53.
- NACCHO (National Aboriginal Community Controlled Health Organisation) & The Royal Australian College of General Practitioners 2018. National guide to a preventive health assessment for Aboriginal and Torres Strait Islander people. Third edition. East Melbourne, Vic.
- O’Grady K, Taylor-Thomson DM, Chang AB, Torzillo PJ, Morris PS, Mackenzie GA et al. 2010. Rates of radiologically confirmed pneumonia as defined by the World Health Organization in Northern Territory Indigenous children. The Medical Journal of Australia 192:592-5.
- Schluger NW & Koppaka R 2014. Lung disease in a global context. A call for public health action. Annals of the American Thoracic Society 11:407-16.
- Torzillo PJ & Chang AB 2014. Acute respiratory infections among Indigenous children. The Medical Journal of Australia 200:559-60.
- WHO (World Health Organization) 2003. WHO Framework Convention on Tobacco Control. Geneva, Switzerland.
- Yashadhana A, Pollard-Wharton N, Zwi A & Biles B 2020. Indigenous Australians at increased risk of COVID-19 due to existing health and socioeconomic inequities. Lancet Regional Health Western Pacific 1.

