Key facts
In 2018–19:
Why is it important?
Having a usual primary health care provider is associated with good communication between the patient and provider, greater levels of trust and satisfaction with providers and better health outcomes for patients (Mainous et al. 2001; Schers et al. 2005; Starfield 1998; Starfield & Shi 2004). Primary care includes care provided through nurses, allied health professionals, midwives, pharmacists, dentists and Aboriginal and Torres Strait Islander health workers. In Australia, general practice is the foundation of primary care (DoH 2018a). Almost 90% of Australians see a general practitioner (GP) at least once each year (RACGP 2019).
Indigenous Australians’ understanding of health is holistic, and includes not just physical wellbeing but also the social, emotional and cultural wellbeing of the whole community (NAHSWP 1989). The concept of health and wellbeing for Indigenous Australians incorporates broader issues including social justice and equity, as well as recognition of the importance of connection to land, culture, spirituality and ancestry and how these affect the individual (DoH 2013). Accessible and appropriate health care for Indigenous Australians should, therefore, deliver care that is cognisant of these broader social and cultural determinants of health.
Indigenous-specific primary health care services, are funded primarily to provide culturally appropriate care for Indigenous Australians. These services are sometimes referred to as Aboriginal Medical Services (AMS). A subset of these services are Aboriginal Community Controlled Health Services (ACCHSs), which are services initiated, operated and controlled by the local Indigenous community to deliver holistic, person-centred, comprehensive and culturally appropriate health care with a locally elected Board of Management (NACCHO). ACCHSs operate in over 140 urban, regional and remote areas across Australia and have made important contributions to improving the lives of Indigenous Australians. These services arose in response to Indigenous Australians’ experiences of racism in the health system and the significant financial, cultural and social barriers to accessing health care (Anderson 2006; Bainbridge et al. 2015).
Individuals with a usual primary care provider are more likely to receive care based on guidelines, preventative care and better coordination of care with other providers to meet patient’s needs (Atlas et al. 2009; Forrest & Starfield 1996). Other benefits of having a continuous doctor–patient relationship include improved diagnoses, better medication management, avoidance of repeat tests or other interventions, and fewer hospitalisations, particularly for people with complex health care needs (Hollander et al. 2009). Patients with a usual GP or practice are much more likely to report that they received very good or excellent care (RACGP 2019).
Data findings
Measuring access to health care is complex, as ‘access’ can refer to distance or time taken to travel to services, affordability, and cultural acceptability. Around 4 in 5 Indigenous Australians live in Major cities and regional areas where mainstream health services are typically located. However, these services are not always accessible to Indigenous Australians, for geographic, social and cultural reasons. Indigenous-specific health services are therefore important providers of primary health care services for Indigenous Australians. These health services are administered and run by a combination of ACCHSs, Primary Health Network services (independent primary health care organisations operated by not-for-profit companies), other non-government organisations, and state/territory local health services (AIHW 2015, 2016; DoH 2018b).
Availability of health care services
Availability of health care services varied across Australia. The Australian Institute of Health and Welfare has mapped access to primary health care services, including Indigenous-specific primary health care services (ISPHCS) and other GP-based primary health services relative to the distribution of the Indigenous population. This analysis revealed that:
- Overall, Australian Government-funded ISPHCSs appeared to be well-positioned relative to where Indigenous people lived and where other GP services were located.
- While Remote and Very Remote areas had the most ISPHCS locations per 1,000 Aboriginal and Torres Strait Islander people, these areas also had the highest proportions of people who needed to travel more than one hour to the nearest ISPHCS.
- There were some areas, many located in Remote and Very Remote Queensland and Western Australia, where there was very limited access to both ISPHCSs and GP services in general (AIHW 2015).
Results from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey (Health Survey) based on self-reported data indicate that the proportion of Indigenous Australians who had a locally available doctor or GP was 95% among those living in Major cities compared with 36% in Very remote areas. The proportion of Indigenous Australians who had a locally available AMS or community clinic was highest in Very remote areas at 93%, compared with 54% of Indigenous Australians in Major cities. (Some caution is needed when interpreting these data, as respondents may not clearly distinguish between the different types of services.)
While hospitals are not considered primary health care providers, in some cases, people may go to a hospital if it is more accessible or affordable or if there is a co-located GP clinic.
Hospitals were available in the local area for 82% of Indigenous Australians living in Inner regional areas, compared with 41% of those living in Very remote areas (Table D3.17.2, Figure 3.17.1).
Figure 3.17.1: Available sources of healthcare by type, Indigenous Australians, by remoteness, 2018–19
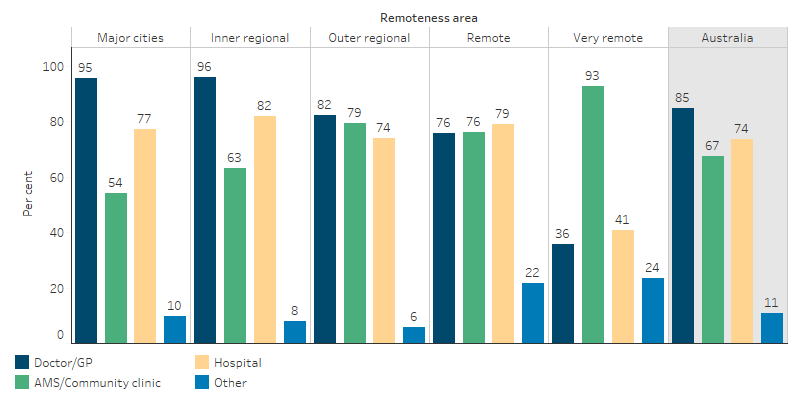
Source: Table D3.17.2. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
Nationally, 4% of Indigenous Australians usually go to hospital if there is a problem with their health (for an analysis of hospitalisations for conditions that could be prevented if primary health care services were better able to meet the needs of Indigenous Australians, see measure 3.07 Selected potentially preventable hospital admissions). A higher use of hospitals for regular health care was reported for Indigenous Australians in Western Australia (8%) and Queensland (6%) than in other jurisdictions (0%–3%) (Table D3.17.1).
Usual source of health care
Based on self-reported data from the 2018–19 Health Survey, 92% of Indigenous people had a usual place to go for health problems and advice:
- 54% usually went to a doctor
- 34% usually went to an AMS or community clinic
- 4% usually went to a hospital
- 0.6% to other health care (including traditional healer).
Use of AMSs and community clinics increased by remoteness—the proportion was lowest in Major cities (15%) and highest in Very remote areas (75%) (Table D3.17.2, Figure 3.17.2).
The usual place that people go for health problems and advice also depends on what services are available, accessible or affordable and the type of health problem.
Figure 3.17.2: Usual source of health-care by type, Indigenous Australians, by remoteness, 2018–19
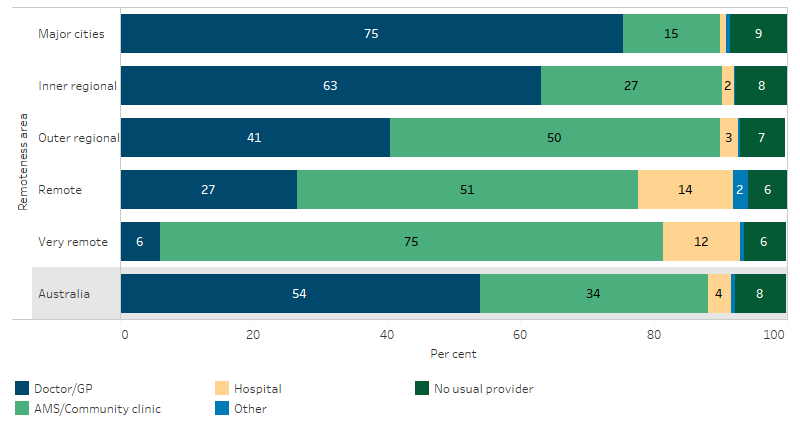
Source: Table D3.17.2. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
Preferred source of care
The Health Survey asked where people would like to go if they were sick or needed advice about their health. In 2018–19, 48% of Indigenous Australians reported they would prefer to go to an AMS or a community clinic, 43% preferred a doctor/GP (other than an AMS or hospital), 7% preferred a hospital and 3% preferred other health care (including a traditional healer).
In most instances Indigenous Australians expressed a preference for the services available in their local area. Preferences varied by remoteness, with doctors/GPs preferred mostly by Indigenous Australians in Major cities (57% compared with 5% in Very remote areas); and AMSs and community clinics preferred mostly by Indigenous Australians in Very remote areas (72% compared with 35% in Major cities) (Table D3.17.2, Figure 3.17.3). Nationally, 20% of Indigenous Australians who said they would like to go to an AMS did not have an AMS available in their local area (Table D3.17.10).
Figure 3.17.3: Preferred source of health-care by type, Indigenous Australians, by remoteness, 2018–19
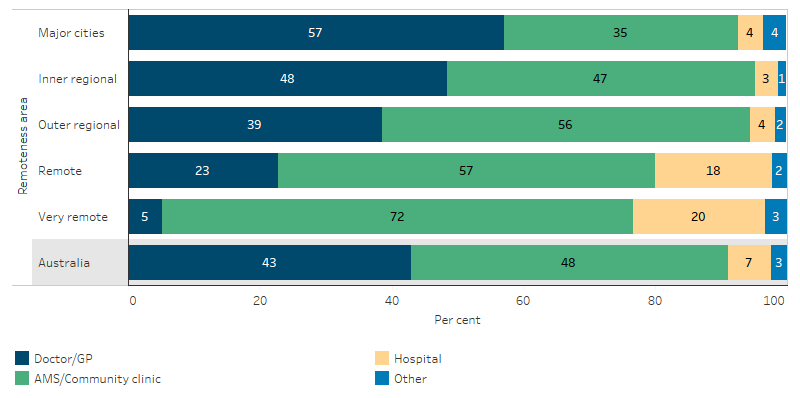
Source: Table D3.17.2. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
Patient experience
In 2018–19, 75% of Indigenous Australians in Non-remote areas rated their health-care experience in the previous 12 months as excellent/very good (Table D3.08.6). Indigenous Australians in Non-remote areas with no usual GP/medical service reported lower rates of satisfaction than those who usually attended a doctor/medical service, with 61% rating their health-care experience in the previous 12 months as excellent/very good, compared with 76% for those with a regular doctor/GP or AMS/community clinic (Table D3.08.8).
The majority of Indigenous Australians aged 15 and over and living in Non-remote areas reported that doctors listened to them (89%), explained things in a way that could be understood (88%), showed respect for what was said (91%) and spent enough time with them (88%) (Table D3.08.8, Figure 3.17.4).
Figure 3.17.4: Patient experience by usual source of health-care, Indigenous Australians aged 15 and over who saw a doctor or specialist (Non-remote), 2018–19
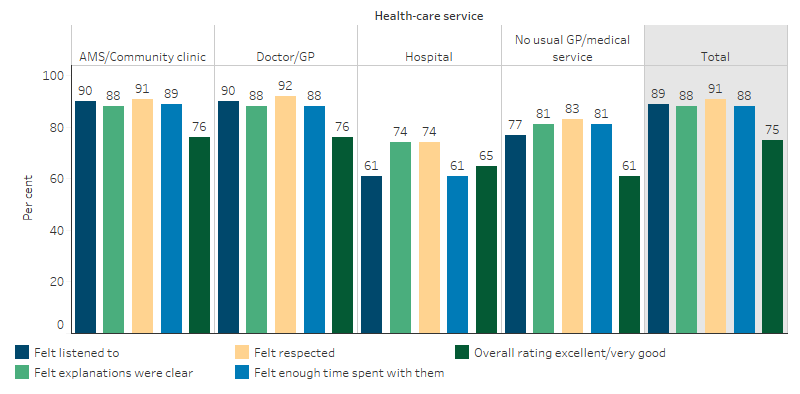
Source: Table D3.08.8. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
National data for all Australians from the Patient Experience Survey 2018–19 showed that GPs always or often listened carefully (92%), showed respect (94%) and spent enough time with their patients (90%) (ABS 2019).
In 2018–19, 23% of Indigenous Australians reported they had been treated unfairly in the previous 12 months because they are Indigenous. Just under 2% of Indigenous people avoided seeking care from doctors, nurses or other staff at hospitals or doctor’s surgeries because of previous unfair treatment (Table D3.08.17).
The 2014–15 National Aboriginal and Torres Strait Islander Social Survey showed that 81% of Indigenous Australians aged 15 and over agreed/strongly agreed that their doctor can be trusted. Further analysis of this issue is discussed in the context of cultural competency (see measure 3.08 Cultural competency, Table D3.08.20).
Research and evaluation findings
Almost 90% of Australians see a GP at least once per year (RACGP 2019). Indigenous Australians, those with lower incomes and people who live outside metropolitan areas visit GPs less, and have more preventable hospital admissions (Swerissen et al. 2018). While mainstream general practice is still a significant source of care for Indigenous Australians, for most GPs, Indigenous Australians make up a small proportion of their clientele. The Bettering the Evaluation and Care of Health (BEACH) program found that for 1.5% of GP encounters the patient identified as Indigenous (2015-16 BEACH Survey). Alternative Indigenous primary health care services have arisen from mainstream services being unable to adequately meet the needs of Indigenous communities (Harfield. et al. 2018; Hayman et al. 2009; RACGP 2019; Spurling et al. 2009).
Primary health care for Indigenous Australians is delivered by a range of providers, including general health service organisations and Indigenous specific organisations. The Indigenous Australians’ Health Programme (IAHP) provides Indigenous Australians with access to primary care services in urban, rural and remote locations, mainly through ACCHS (Swerissen et al. 2018). GPs working in ACCHS report different challenges to GPs working in other environments. Two in five (40%) report difficulty sourcing and retaining high-quality staff (RACGP 2019).
Compared with non-Indigenous Australians, Indigenous Australians face greater barriers in accessing primary care. Using an area-based index of access to GP services relative to the health needs of Indigenous and non-Indigenous Australians, research by the Australian Institute of Health and Welfare (AIHW) suggests that Indigenous Australians experience a pattern of worsening access to GPs relative to need with increasing remoteness (AIHW 2014). This is attributed to relatively poor access to GPs and relatively high predicted need for primary health care in more remote areas. The pattern is less dramatic for non-Indigenous Australians, as those living in Very remote areas are more likely to live in areas with higher access to GPs than Indigenous Australians (AIHW 2014).
Further research by the AIHW found that Remote and Very remote areas have the most ISPHCS funded by the Australian Government per 1,000 Indigenous Australians. However, these areas also had the highest proportion of Indigenous Australians needing to travel over one hour to access the nearest Indigenous specific primary health care service. Forty Statistical Area Level 2s (medium-sized regions with between 3,000 and 25,000 people) were identified as service gap areas with no Indigenous specific primary health care service within a one hour drive and with poor access to GP services in general. An analysis showed that 61% of the Statistical Area Level 2s with service gaps have a high rate of potentially preventable hospitalisations (above the median for all Statistical Area Level 2s) (AIHW 2015).
A systematic scoping review identified the characteristics of Indigenous primary health care service delivery models. Culture was the most prominent characteristic that underpinned all of the other seven characteristics that were identified—accessible health services, community participation, continuous quality improvement; culturally appropriate and skilled workforce, flexible approach to care; holistic health care, and self-determination and empowerment (Harfield et al. 2018).
Implications
Most Indigenous Australians have a usual source of health care. This finding is encouraging as access to a usual source of care is one of the foundations for a good primary health care system. The Health Survey data shows that the main sources of primary health care for Indigenous Australians are GPs, AMSs and community clinics. The interpretation of the Health Survey data in this measure requires caution as some respondents may not clearly differentiate between these categories and it is not clear to what degree respondents intended to refer to mainstream health services or Indigenous specific primary health care services.
Although there is a lack of data on mainstream primary health care use, mainstream general practice remains a significant source of care for Indigenous Australians. However, for most GPs, Indigenous clients will remain a small proportion of their client base.
Being able to access health care is widely accepted as fundamental to improving health outcomes. Indigenous Australians face a range of barriers to accessing primary health care, including discrimination, racism and poor communication with health professionals. Measure 3.08 Cultural competency provides further exploration of the need for mainstream services to develop cultural competency in order to provide culturally appropriate care to Indigenous Australian clients. However, there are limited data available on the cultural competency of health services (Paradies et al. 2014) and on the effectiveness of interventions to address cultural competency in health care for Indigenous Australians (Clifford et al. 2015; Truong et al. 2014). In particular, there remains a lack of reporting on the policies and practices of mainstream health services (AIHW 2019).
Evidence shows that access to primary health care can be improved for Indigenous Australians if services are owned and managed by Indigenous communities. ACCHSs are a vital part of Australia’s health care system and many Indigenous Australians prefer these services, particularly those living in Very Remote areas (Campbell et al. 2018).
The policy context is at Policies and strategies.
References
- ABS (Australian Bureau of Statistics) 2019. Patient Experiences in Australia: Summary of Findings, 2018-19. Cat. no. 4839.0. Canberra: ABS.
- AIHW (Australian Institute of Health and Welfare) 2014. Access to primary health care relative to need for Indigenous Australians. Canberra: AIHW.
- AIHW 2015. Spatial variation in Aboriginal and Torres Strait Islander people's access to primary health care. Canberra: AIHW.
- AIHW 2016. Australia's health 2016. Canberra: AIHW.
- AIHW 2019. Cultural safety in health care for Indigenous Australians: monitoring framework. Canberra: Australian Institute of Health and Welfare.
- Anderson I 2006. Aboriginal Health and Welfare Colonialism: 1967-2004. La Trobe University.
- Atlas SJ, Grant RW, Ferris TG, Chang Y & Barry MJ 2009. Patient-physician connectedness and quality of primary care. Annals of Internal Medicine 150:325-35.
- Bainbridge R, McCalman J, Clifford A & Tsey K 2015. Cultural competency in the delivery of health services for Indigenous people. Issues paper no. 13. Closing the Gap Clearinghouse. Canberra: Australian Institute of Health and Welfare & Australian Institute of Family Studies.
- Campbell MA, Hunt J, Scrimgeour DJ, Davey M & Jones V 2018. Contribution of Aboriginal Community-Controlled Health Services to improving Aboriginal health: an evidence review. Australian Health Review 42:218-26.
- Clifford A, McCalman J, Bainbridge R & Tsey K 2015. Interventions to improve cultural competency in health care for Indigenous peoples of Australia, New Zealand, Canada and the USA: a systematic review. International Journal for Quality in Health Care 27:89-98.
- DoH (Australian Government Department of Health) 2013. National Aboriginal & Torres Strait Islander Health Plan 2013-2023. Canberra: Commonwealth of Australia.
- DoH 2018a. Fact Sheet: Primary Health Care.
- DoH 2018b. Fact Sheet: Primary Health Networks.
- Forrest CB & Starfield B 1996. The effect of first-contact care with primary care clinicians on ambulatory health care expenditures. Journal of Family Practice 43:40-8.
- Harfield. SG, Davy. C, McArthur. A, Munn. Z, Brown. A & Brown. N 2018. Characteristics of Indigenous primary health care service delivery models: a systemic scoping review. Globalization and Health 14.
- Hayman NE, White NE & Spurling GK 2009. Improving Indigenous patients’ access to mainstream health services: the Inala experience. The Medical Journal of Australia 190:604-6.
- Hollander MJ, Kadlec H, Hamdi R & Tessaro A 2009. Increasing value for money in the Canadian healthcare system: new findings on the contribution of primary care services. Healthcare Quarterly 12:32-44.
- Mainous AG, 3rd, Baker R, Love MM, Gray DP & Gill JM 2001. Continuity of care and trust in one's physician: evidence from primary care in the United States and the United Kingdom. Family Medicine 33:22-7.
- NACCHO (National Aboriginal Community Controlled Health Organisation)
- NAHSWP (National Aboriginal Health Strategy Working Party) 1989. National Aboriginal Health Strategy.
- Paradies Y, Truong M & Priest N 2014. A systematic review of the extent and measurement of healthcare provider racism. Journal of General Internal Medicine 29:364-87.
- RACGP (The Royal Australian College of General Practitioners) 2019. General Practice: Health of the Nation 2019. East Melbourne, Vic.
- Schers H, van den Hoogen H, Bor H, Grol R & van den Bosch W 2005. Familiarity with a GP and patients' evaluations of care. A cross-sectional study. Family Practice 22:15-9.
- Spurling G, Hayman NE & Cooney AL 2009. Adult health checks for Indigenous Australians: the first year's experience from the Inala Indigenous Health Service. The Medical Journal of Australia 190:562-4.
- Starfield B 1998. Primary Care: Balancing Health Needs, Services and Technology. New York: Oxford University Press.
- Starfield B & Shi L 2004. The medical home, access to care, and insurance: a review of evidence. Pediatrics 113:1493-8.
- Swerissen H, Duckett S & Moran G 2018. Mapping primary care in Australia. Victoria, Australia: Grattan Institute.
- Truong M, Paradies Y & Priest N 2014. Interventions to improve cultural competency in healthcare: a systematic review of reviews. BMC health services research 14:99.

