|
Caveat for users A review of the method for allocating expenditure on medications by Indigenous status has revealed that the current estimates understate pharmaceutical expenditure for First Nations people. Consequently, the data do not accurately reflect the total pharmaceutical expenditure for First Nations people. A new method has been identified, and work on producing updated estimates is underway. The updates to the measure are anticipated for publication in 2025. |
Why is it important?
Essential medicines save lives and improve health when they are available, affordable, quality-assured and properly used (WHO 2017). The World Health Organization policy framework on medicines states that essential medicines are intended to be available ‘at all times in adequate amounts, in the appropriate dosage forms, with assured quality and adequate information and at a price the individual and community can afford’ (WHO 2004). Affordable access to medicines is important for many acute and chronic illnesses. For chronic illnesses such as diabetes, hypertension, heart disease and renal failure, multiple medications may be required for many years to avoid complications (WHO 2017). It is important to ensure that Aboriginal and Torres Strait Islander people, who experience high rates of acute and chronic illnesses, can access appropriate prescription medications when they are required.
In Australia, the main mechanism for ensuring reliable, timely and affordable access to a wide range of prescription medications is the Australian Government’s Pharmaceutical Benefits Scheme (PBS) and the Repatriation Pharmaceutical Benefits Scheme (RPBS—for eligible Department of Veterans’ Affairs beneficiaries). In 2018–19, the PBS subsidised the cost of 205.1 million prescriptions, at the cost of approximately $11.82 billion (DoH 2019).
As noted in the National Medicines Policy, cost should not be a substantial barrier to people’s access to medicines they need. Therefore, normal market mechanisms may be tempered in access arrangements, to increase the affordability of important medicines. For example, the PBS facilitates access to certain prescribed medicines by subsidising costs, and subsidies also occur when hospitals supply medicines to patients. However, such subsidies are not costless, and the community as a whole must bear them (DoH 2014a).
To address barriers to access to PBS medicines by people living in remote areas of Australia, who may have limited access to prescribers and community pharmacies, the Australian Government established the Remote Area Aboriginal Health Services (RAAHS) Program under section 100 of the National Health Act 1953. Under these arrangements, patients of approved RAAHS can obtain eligible medicines at the time of consultation, without a PBS prescription and at no cost.
The Closing the Gap (CTG) PBS Co-payment Measure (the CTG Measure) is available to Aboriginal and Torres Strait Islander people of any age who present with, or are at risk of chronic disease, and who:
- would experience setbacks in the prevention or ongoing management of chronic disease if the person did not take the prescribed medicine
- are unlikely to adhere to their medicines regimen without assistance through the program (DoH 2020a).
Eligible patients can be registered at either:
- general practices participating in the Practice Incentives Program—Indigenous Health Incentive (PIP IHI)
- Aboriginal and Torres Strait Islander Health Services in urban and rural settings.
Although the CTG Measure is focused on non-remote areas, it is available in remote areas through general practices participating in the PIP where there is a pharmacy available to dispense prescriptions. However, this is complemented by the RAAHS so that in remote areas where there is no pharmacy, patients can access PBS medicines through the approved Aboriginal Health Service (DoH 2014b).
The Australian Government also contributes to the cost of PBS medicines supplied to outpatients and patients upon discharge from public hospitals in most jurisdictions, excluding New South Wales and the Australian Capital Territory, through the Pharmaceutical Reform Agreements (PRAs). Patients are required to pay a patient contribution, which is not linked to the CTG Measure. However, many public hospitals choose to waive the applicable co‑payment for Indigenous Australians.
Data findings
Expenditure
In 2015–16, the total expenditure on pharmaceuticals in Australia for Indigenous Australians was $420 million, which was an average of $537 per person. For non-Indigenous Australians, the average expenditure was $891 per person (Table D3.15.1, Figure 3.15.1).
Figure 3.15.1: Directly administered expenditure by the Australian Government, non-government organisations and individuals on the Pharmaceutical Benefit Scheme, by Indigenous status, 2015–16
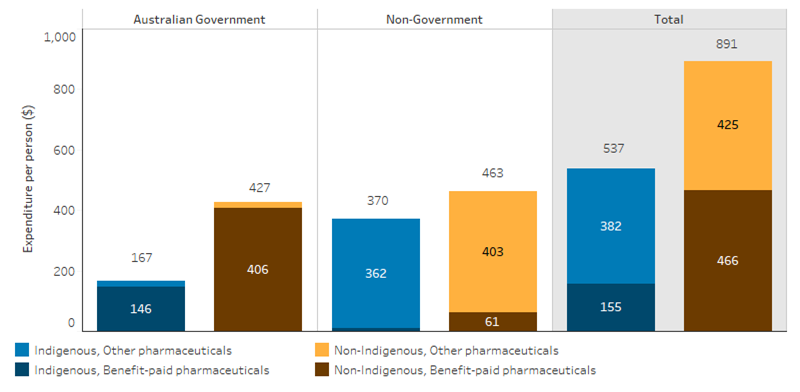
Source: Table D3.15.1. AIHW Health Expenditure database.
Expenditure by the Australian Government, through the PBS and the RPBS, accounted for 31% of total pharmaceutical expenditure for Indigenous Australians and 48% for non-Indigenous (Table D3.15.1). This represents an average expenditure by the Australian Government of $167 per person for Indigenous Australians compared with $427 per person for non-Indigenous (Table D3.15.2, Figure 3.15.2).
For Indigenous Australians, Australian Government pharmaceutical expenditure via mainstream PBS (excluding section 100 expenditure) accounted for 61% of PBS expenditure. Section 100 expenditure (where medications are distributed through Aboriginal and Torres Strait Islander Health Services) accounted for 19% (Table D3.15.2, Figure 3.15.2). The RPBS accounted for less than 1% of expenditure.
Figure 3.15.2: Australian Government expenditures through the Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Scheme (RPBS), by Indigenous status, 2015–16
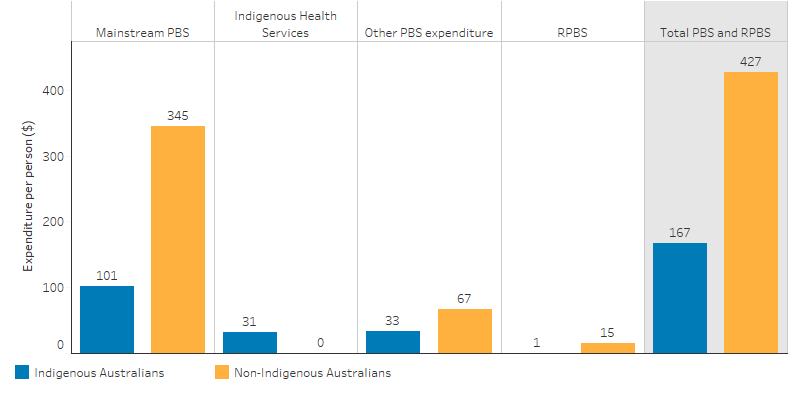
Source: Table D3.15.2. AIHW Health Expenditure database.
In 2015–16, expenditure per person through the mainstream PBS (excluding RPBS and other Australian Government expenditure) for Indigenous Australians was highest in Remote and Very Remote areas ($241), followed by Inner and Outer regional areas ($130) and Major cities ($116). The gap between PBS expenditure per person for Indigenous and non-Indigenous Australians was greatest in Major cities and Inner/Outer regional areas (Table D3.21.8, Figure 3.15.3).
Figure 3.15.3: Australian Government expenditure through the Pharmaceutical Benefits Scheme (PBS) per person, Indigenous and non-Indigenous Australians, by remoteness area of patient’s residence, 2015–16
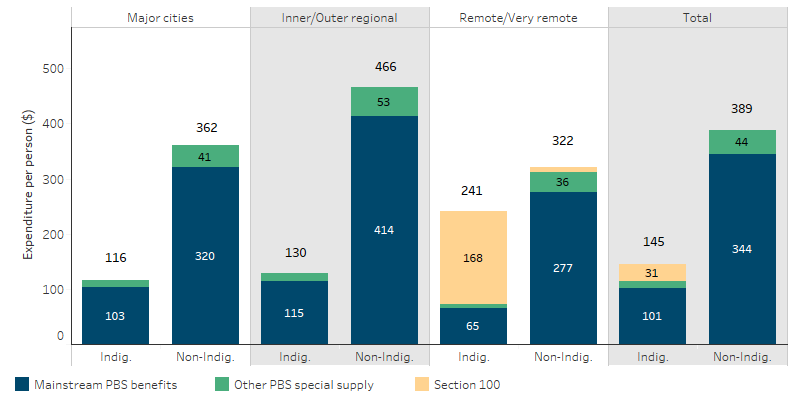
Note: Data in table D3.21.8 excludes Repatriation Pharmaceutical Benefits Scheme (RPBS) and other Australian Government expenditure and is not comparable to HPF Tables D3.15.1, D3.15.2 and D3.15.3.
Source: Table D3.21.8. AIHW Health expenditure database.
Between 2010–11 and 2016–17, expenditure on pharmaceuticals covered by the mainstream PBS and the RPBS grew for Indigenous Australians by 3.7% per year in real terms and by 2.8% for non-Indigenous Australians (Table D3.15.4, Figure 3.15.4). In 2016–17, average PBS expenditure per person for Indigenous Australians was estimated to be 29% of the amount spent for non-Indigenous Australians. This ranged from 22% in 2011–12 and 34% in 2014–15 (Table D3.15.4).
Figure 3.15.4: Australian Government expenditure on mainstream Pharmaceutical Benefits Scheme (PBS) and Repatriation Pharmaceutical Scheme (RPBS) (constant prices) per person, by Indigenous status, 2010–11 to 2016–17
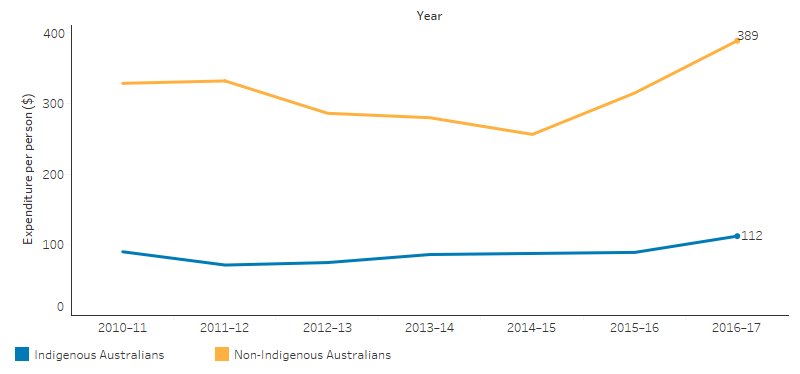
Source: Table D3.15.4. AIHW Health Expenditure database.
Having prescriptions filled
Results from the 2018–19 National Aboriginal and Torres Strait Islander Health Survey showed that 86% of Indigenous Australians aged 15 and over had their prescriptions filled in the last 12 months. This increased from the 81% that was reported in the 2012–13 Australian Aboriginal and Torres Strait Islander Health Survey (Table D3.15.5, HPF 2017 Table 3.15.5). Indigenous males were more likely than Indigenous females to fill their prescriptions (89% compared with 83%, respectively). The most common reasons reported by Indigenous Australians for not having a prescription filled in the last 12 months were because of cost (36%), they decided they didn’t need it (30%), they didn’t want to (15%) or they were too busy (11%) (Table D3.15.5).
Indigenous pharmacist workforce
In 2017, of the 24,609 pharmacists nationally, 70 (0.3%) were Indigenous. The number of full-time equivalent Indigenous pharmacists declined with remoteness. The rate was highest in Major cities (13 per 100,000), lower in Inner and Outer regional areas combined (6.7 per 100,000) and was lowest in Remote and Very remote areas combined (3.3 per 100,000) (Table D3.12.5).
Research and evaluation findings
Results from one study show a reduction in hospitalisations for chronic conditions in areas with higher uptake of the CTG Measure (Trivedi et al. 2016). A multi-system coordinated approach to the management of chronic conditions, including clinical care programs is necessary for improving access to health care and reducing chronic disease (Bailie et al. 2015; Reed 2017).
There have been multiple reviews of the RAAHS program and the CTG Measure over the years. Although the programs have improved access to low or no cost PBS medicines for Indigenous Australians, there remain gaps between the programs. In particular, the geographic basis for eligibility to the programs, combined with the restrictions on who can register patients for the CTG Measure and issue CTG prescriptions, hinders the programs from contributing optimally to close the gap in health outcomes.
For example, hospital-based prescribers are unable to provide CTG prescriptions unless they are a specialist treating a patient who has been referred by a general practitioner working out of a general practice participating in the PIP IHI.
The Independent Review of Pharmacy Remuneration and Regulation published in 2017 provided recommendations on future remuneration, regulation and other arrangements that apply to pharmacy and wholesalers for the dispensing of medicines and services offered under the PBS. The review aimed to ensure that there is continued reliable and affordable access to medicines listed on the PBS to Australians who need them, regardless of their location (King et al. 2017).
The review included recommendations to ensure access to PBS Medicines and community pharmacy services for Indigenous Australians. These included improved access to medicines programs for Indigenous Australians, particularly in rural areas; pharmacy ownership and operation by Aboriginal health services; and appropriate labelling of medicines for patients, including training for Aboriginal health services and pharmacies in remote areas to mitigate risks associated with remote and bulk supply (King et al. 2017). In response to the review, the Australian Government is considering these recommendations in the context of other policies and programs that aim to improve access to PBS medicines for Indigenous Australians (DoH 2018a).
Implications
There is a large gap between PBS pharmaceutical expenditure for Indigenous and non‑Indigenous Australians. In 2016–17, the average PBS expenditure per person for Indigenous Australians was estimated to be 29% of the amount spent for non-Indigenous Australians. Further, Indigenous Australians experience a burden of disease and injury 2.3 times as high as non‑Indigenous Australians and as such the level of pharmaceutical expenditure would be expected to be higher in order to meet that need. While there is some evidence of improved access to medicines and improved outcomes, more effort is required to ensure Indigenous Australians are able to benefit from access to the medicines they need.
As estimation of the gap between Indigenous and non-Indigenous Australians and the level commensurate with need is complicated by the absence of high-quality data sources on Indigenous pharmaceutical usage and expenditures, such as a lack of patient level data. For example, there may be some instances of medicines being dispensed in services that are not captured in the PBS data.
To provide effective health care to Indigenous Australian patients, there is a need to address barriers to accessing and the under-use of prescription medicines such as financial barriers (despite safety net schemes), availability and location of services (primary health care, specialists and pharmacies), language barriers and the cultural competency of services (DoH 2018b).
The Pharmaceutical Society of Australia’s Guide to Providing Pharmacy Services to Aboriginal and Torres Strait Islander People was released in 2014 to assist pharmacists and pharmacy staff to be responsive to health beliefs, practices, culture and linguistic needs of Indigenous Australians, families and communities. The guide encourages increased engagement with Indigenous health services and key Indigenous organisations, includes an overview of Indigenous specific medicine programs and provides a resource list from which pharmacists can gather more in-depth information (Pharmaceutical Society of Australia 2014).
Under the Sixth Community Pharmacy Agreement (2015–20) the Australian Government provided funding to support a pharmacy trial program to identify community pharmacy programs that improve clinical outcomes for patients and/or utilise the full scope of a pharmacist’s role in delivering primary health care services. These trials included the Improved Medication Management for Aboriginal and Torres Strait Islanders Feasibility Study (IMeRSe Feasibility Study) and Integrating practice pharmacists into Aboriginal Community Controlled Health Services (the IPAC Project) (DoH 2015).
On 12 June 2020, the Australian Government announced the Seventh Community Pharmacy Agreement, which includes a commitment to enhancing the CTG Measure to:
- enable Indigenous Australian patients to register for the CTG Measure, regardless of where they live and their chronic disease status
- expand the range of health care professionals who can register patients for the CTG Measure and issue CTG prescriptions (DoH 2020b).
The policy context is at Policies and strategies.
References
- Bailie J, Schierhout G, Laycock AF, Kelaher M, Percival N, O’Donoghue LR et al. 2015. Determinants of access to chronic illness care: a mixed-methods evaluation of a national multifaceted chronic disease package for Indigenous Australians. BMJ Open 5.
- DoH (Australian Government Department of Health) 2014a. National Medicines Policy.
- DoH 2014b. Closing the gap pbs co-payment measure. Canberra: Australian Government Department of Health,.
- DoH 2015. Pharmacy trial programme.Canberra: Australian Government Department of Health,
- DoH 2018a. Australian Government Response to the Review of Pharmacy Remuneration and Regulation. (ed., Health Do). Canberra.
- DoH 2018b. PBS Section_1_2_Explanatory Notes, Improving the capacity of the PBS to meet particular Aboriginal and Torres Strait Islander health needs.
- DoH 2019. PBS Expenditure and Prescriptions Report 1 July 2018 to 30 June 2019.
- DoH 2020a. The Closing The Gap - PBS Co-payment Measure.
- DoH 2020b. New (7th) Community Pharmacy Agreement. Canberra: Australian Government Department of Health,.
- King S. et al. 2017. Review of Pharmacy Remuneration and Regulation–Final Report. (ed., Health Do). Canberra: Department of Health.
- Pharmaceutical Society of Australia 2014. Guide to providing pharmacy services to Aboriginal and Torres Strait Islander people. Canberra: PSA.
- Reed M 2017. Reducing Out-of-Pocket Costs to Coordinate Prescription Medication Benefit Design with Chronic Disease Outreach and Clinical Care. Journal of General Internal Medicine.
- Trivedi AN, Bailie R, Bailie J, Brown A & Kelaher M 2016. Hospitalizations for Chronic Conditions Among Indigenous Australians After Medication Copayment Reductions: the Closing the Gap Copayment Incentive. Journal of General Internal Medicine.
- WHO (World Health Organization) 2004. WHO Policy Perspectives on Medicines. Geneva: WHO.
- WHO 2017. Towards access 2030: WHO essential medicines and health products strategic framework 2016-2030. WHO.

