Key messages
- Between 2009–10 and 2018–19, the rate of Aboriginal and Torres Strait Islander people accessing Indigenous-specific health assessments through the Medicare Benefits Schedule increased from 68 checks per 1,000 population to 297 per 1,000 population.
- The age-standardised proportion of Indigenous women aged 50–69 who were screened for breast cancer increased from 29% in 2010–2011 to 38% in 2018–2019, before dropping to 35% in 2019–2020, most likely due to the impact of the COVID-19 pandemic from March 2020.
- Data for December 2018 indicated that 43% of eligible Indigenous female regular clients aged 20–74 attending Indigenous-specific primary health-care services had a cervical screening test (Pap test or an HPV test) in the previous five years.
- In 2019–2020, the participation rate in the National Bowel Cancer Screening Program for Indigenous Australians aged 50–74 was estimated to be 35%,11 percentage points lower than non-Indigenous Australians (46%).
- Data from the National Bowel Cancer Screening Program show Indigenous participants were more likely to receive a positive result, indicating potential cancer, than non-Indigenous participants (9.9% and 6.9%, respectively). However, Indigenous participants with a positive result had a lower rate of follow-up colonoscopy (51% compared with 62%) and a longer median time between a positive screen and assessment (64 days compared with 49, days respectively).
Why is it important?
Early detection is the discovery of a disease or condition at an early stage of its development or onset, usually before symptoms occur. Early detection may occur through individual patient care or screening programs for targeted populations. Screening is the recognition or diagnosis of an unrecognised disease or condition in the general population by using reliable tests, examinations or other procedures that can be applied rapidly (Zwar & Ackermann 2016). Early treatment is the provision of a treatment regime following as soon as possible after the detection and confirmatory diagnosis of disease. Early detection and treatment programs are most effective when there are systematic approaches to ensuring that assessment and screening occur regularly and at recommended intervals.
Detecting and treating disease early is both more effective and more efficient than treating more advanced disease. For some diseases, early detection and treatment can result in a cure, while for others, it may slow the onset of the disease and reduce the risk of death.
Screening programs need to meet a range of criteria to ensure their efficacy and acceptability to the public. They also need to promote equity of access for all members of the target population, including important subgroups such as Aboriginal and Torres Strait Islander people and people from culturally and linguistically diverse backgrounds (Clinical Principal Committee Standing Committee on Screening 2018).
In Australia, primary health care providers, including Aboriginal and Torres Strait Islander health services and general practitioners (GPs), have a crucial role in detecting and treating disease in its early stages. The World Bank includes selected early detection and management of non-communicable diseases (for example, screening programs) as one of the seven recommended cost‑effective health interventions that can be delivered in the primary health care setting and that play a key role in avoiding adverse health outcomes (Jamison et al. 2017; Jamison et al. 1993).
The Australian Government provides GP health assessments and checks for Indigenous Australians under the Medicare Benefits Schedule (MBS), along with follow-up care and incentive payments for improved chronic disease management and cheaper medicines through the Pharmaceutical Benefits Scheme (PBS). The MBS Item 715 is a general health assessment for Indigenous Australians and is used for detecting a wide range of potential health issues that may need follow-up care such as high blood pressure, high sugar levels, oral health, mental health, sexual health, immunisation status, hearing and vision.
National cancer screening programs are designed to reduce illness and death through early detection of cancer or pre-cancerous abnormalities. National programs for breast and cervical screening were implemented in Australia in the early 1990s. The National Cervical Screening Program (NCSP) currently recommends that asymptomatic women aged 25 to 74 should have a cervical screening test every five years (DoH 2020a). BreastScreen Australia recommends two-yearly screening for women aged 50–74 (DoH 2020b). The National Bowel Cancer Screening Program (NBCSP) began in 2006, and biennial screening for males and females aged 50 to 74 is recommended (DoH 2020c).
The National Aboriginal and Torres Strait Islander Health Plan 2021-2031 (the Health Plan), released in December 2021, provides a strong overarching policy framework for Aboriginal and Torres Strait Islander health and wellbeing. The Health Plan was developed in genuine partnership with Aboriginal and Torres Strait Islander leaders.
‘Priority Five’ of the Health Plan focuses on early intervention approaches that are accessible to Aboriginal and Torres Strait Islander people and provide timely, high quality, effective, culturally safe and responsive care. The Health Plan includes a focus on the conditions that disproportionately impact Indigenous Australians as a way to close the gap in health outcomes and ensure access to screening and follow-up care, when and where they are required. The Health Plan emphasises place-based early intervention approaches that are determined locally.
The Health Plan is discussed further in the Implications section of this measure.
Data findings
Health checks
Health checks through MBS health assessment items for Indigenous Australians aged 55 and over were introduced in 1999, for those aged 15–54 in 2004, and in 2006 for those aged 0–14. In 2009–10, measures to increase take-up of health assessments by those aged 15 and over were introduced.
In 2018–19, a total of 81,637 health assessments were undertaken for children aged 0–14, representing 29% of Indigenous children. There were 127,798 health assessments provided for Indigenous Australians aged 15–54 (representing 28% of this population) and 39,406 for those aged 55 and over (representing 40% of this population) (Table D3.04.1).
For Commonwealth-funded Indigenous primary health care organisations, 37% of Indigenous children 0–4 (who were regular clients) had received an MBS health assessment in the 12 months prior to December 2018. For eligible adults who were regular clients, 50% of those aged 25–54 had received a health check in the previous 24 months, as had 58% of those aged 55 and over (Table D3.04.25).
Cancer screening
Indigenous Australians are less likely to participate in breast, cervical and bowel population screening programs than non-Indigenous Australians. This section provides information on cancer screening participation rates based on available data, noting there are limitations in the data used for calculating the screening participation rates for Indigenous Australians due to under-reporting of Indigenous status.
Breast screening
BreastScreen Australia is a joint initiative of the Australian and state and territory governments and offers a free mammogram every two years for women aged 40 and over, and actively invites women aged 50–74.
The latest BreastScreen Australia data (2-year period between 2019–2020) showed that after adjusting for differences in the age structure between the two populations, 36% of Indigenous Australian women aged 50–74 had been screened. This was 14 percentage points lower than for non-Indigenous women (50%) (Table D3.04.9).
Breast cancer screening participation rates for Indigenous women aged 50–74 were lower in remote areas (23% in Very remote areas, and 28% in Remote areas) than in non-remote areas (36% in Major cities, 41% in Inner regional areas, and 38% in Outer regional areas) (Table D3.04.30). Screening participation rates for Indigenous women aged 50–74 also varied by states and territories, with the lowest rate in the Northern Territory (18%) and the highest in Queensland (44%) (Table D3.04.9).
The 2018–19 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS) showed that 85% (48,660) of Indigenous women aged 50–69 reported having at least one mammogram (Table D3.04.10).
Cervical screening
Under the former National Cervical Screening Program (NCSP) (until 1 December 2017), Pap tests were recommended every two years for most women aged 18–69. Under the renewed NCSP, the cervical screening test (CST) replaced the Pap test in 2017—a human papillomavirus (HPV) test, followed by a cytology test if HPV is found—is recommended every five years for most women aged 25–74.
An estimated 56% of all Australian women aged 25–74 had an HPV test under the renewed NCSP over the three years between 2018–2020. However, 28% of all women aged 25–74 who had a HPV test under the National Cervical Screening Program in 2018–2020 did not state their Indigenous status. This high level of incomplete Indigenous identification in the National Cancer Screening Register makes it challenging to estimate the cervical screening participation rate by Indigenous women accurately, and so a participation rate is not available (AIHW 2021a).
Reported data from the 2018–19 NATSIHS showed that 50% (105,100) of Indigenous women aged 20–69 had cervical screening at least every two years (Pap test or HPV test). Proportions varied by remoteness area, from 41% in Inner regional areas to 57% in Very remote areas (Table D3.04.15, Table D3.04.16, Figure 3.04.1).
Figure 3.04.1: Indigenous women aged 20–69 reporting whether had cervical screening at least every 2 years (Pap test or HPV test), by remoteness, 2018–19
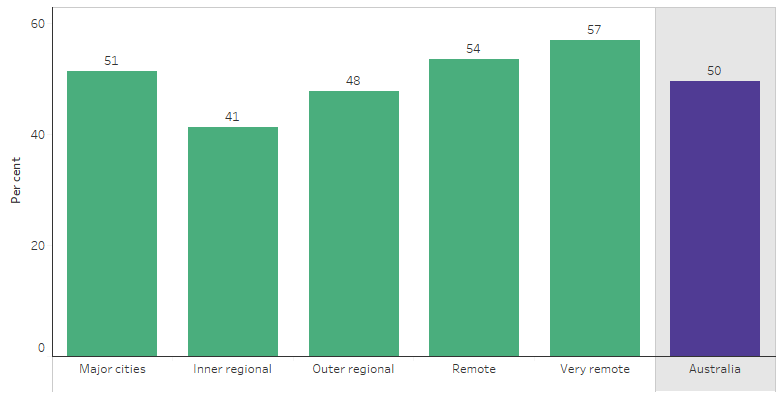
Source: Table D3.04.15. AIHW and ABS analysis of National Aboriginal and Torres Strait Islander Health Survey 2018–19.
As of December 2018, Commonwealth-funded Indigenous-specific primary health care organisations reported that 26% (29,140) of regular female clients aged 20–74 had a cervical screening (Pap test or HPV test) in the previous two years, 34% (38,690) in the previous three years and 43% (48,510) in the previous five years (Table D3.04.27).
The proportion of Indigenous female regular clients of the Commonwealth-funded Indigenous-specific primary health care organisations who were aged 20–74 and had cervical screening in the previous five years varied by remoteness, from 36% in Outer regional areas to 52% in Very remote areas. Proportions also varied by jurisdiction from 35% in New South Wales, and the Australian Capital Territory combined, to 56% in the Northern Territory (Table D3.04.27, Table D3.04.28).
National Bowel Cancer Screening Program
Data from the 2018–19 NATSIHS indicates that, based on self-reported, 23% (13,600) of Indigenous males and 20% (12,800) of Indigenous females aged 50–74 had at least one bowel cancer screening test (Table D3.04.17).
Over the period January 2019 to December 2020, a total of 2,523,538 Australians returned a valid screening test in the National Bowel Cancer Screening Program (NBCSP); of these, 14,296 identified as Indigenous (0.6%).
To determine participation rates by Indigenous status, the number of screening invitations sent out by Indigenous status is also needed. At present, this information isn’t available, so must be estimated. To estimate the number of invitations sent out to Indigenous Australians, the percentages of those aged 50–74 who reported being Indigenous in the 2016 Census was applied to the number of overall invitations (by age group and sex) (see Appendix F of AIHW 2021b).
The estimated participation rate in the NBCSP for Indigenous Australians aged 50–74 was 35% in 2019–2020. This was 11 percentage points lower than the estimated participation rate of 46% for non-Indigenous Australians. Given the limitations in the data available to estimate Indigenous Australians’ participation in the NBCSP, caution should be used when interpreting these data (see Appendix F of AIHW 2021b).
In 2019, Indigenous participants were more likely to receive a positive (that is, potentially abnormal) Immunochemical faecal occult blood test (iFOBT) result than non-Indigenous participants (10% and 7%, respectively). However, Indigenous participants with a positive result had a lower rate of follow-up colonoscopy (51% compared with 62%) and a longer median time between a positive screen and assessment (64 days compared with 49 days, respectively) (AIHW 2021b) (Table 3.04-1).
Table 3.04-1: Summary of National Bowel Cancer Screening Program screening, results and assessments, people aged 50–74, by Indigenous status, 2019
|
Number |
Indigenous |
Non-Indigenous |
|---|---|---|
|
Screened |
12,214 |
1,245,454 |
|
Positive iFOBT result |
1,185 |
83,440 |
|
Diagnostic assessment (colonoscopy) |
516 |
52,084 |
|
Rates (%) |
Indigenous |
Non-Indigenous |
|---|---|---|
|
iFOBT positivity rate |
9.7 |
6.7 |
|
Diagnostic assessment rate |
43.5 |
62.4 |
|
Time between positive screen and assessment (days) |
Indigenous |
Non-Indigenous |
|---|---|---|
|
Median |
62 |
49 |
|
90th percentile |
157 |
139 |
Source: AIHW 2021b. National Bowel Cancer Screening Program: monitoring report 2021.
Other cancer screening
The 2018–19 NATSIHS showed that 58% (36,600) of Indigenous males aged 50 and over reported having been tested for prostate cancer at least once (Table D3.04.19). Of Indigenous adults, 7.4% (35,820) had been tested at least once for skin cancer, and 1.5% (7,260) had participated in a lung cancer screening test (Table D3.04.18).
Change over time
Health checks
Between 2009–10 and 2018–19, the number of Indigenous Australians accessing Indigenous-specific health assessments through the MBS increased by about fivefold, from 47,283 Indigenous patients to 248,841 Indigenous patients. The rate of MBS health assessments increased for Indigenous Australians from 68 per 1,000 to 297 per 1,000 over the years from 2009–10 to 2018–19. A relatively large annual increase in health assessments for Indigenous Australians was seen between 2009–10 and 2010–11 (48%) (Table D3.04.3, Figure 3.04.2).
Figure 3.04.2: Rate of MBS health checks/assessments for Indigenous Australians (MBS item 715), by age group, 2006–07 to 2018–19
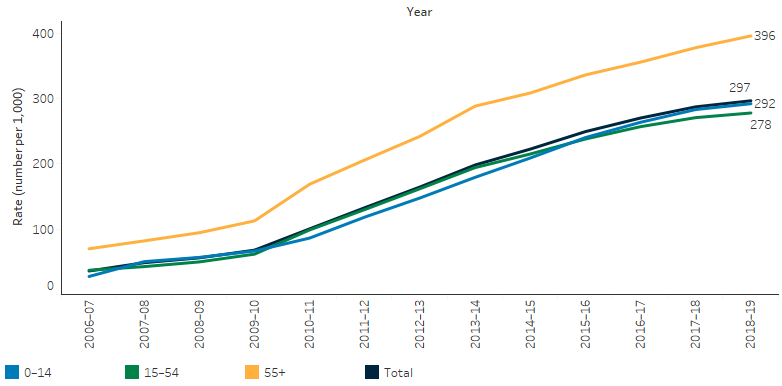
Source: Tables D3.04.3, D3.04.5, D3.04.6, D3.04.7. AIHW analysis of Department of Health Medicare claims data.
Breast cancer screening
Between 2006–2007 and 2010–2011, participation rates in BreastScreen Australia among Indigenous women aged 40 and above remained at around 18%. In the subsequent decade between 2010–2011 and 2018–2019, participation rates among Indigenous women aged 40 and above increased from 18% to 27%, before decreasing to 25% in 2019–2020, most likely due to the impact of the COVID-19 pandemic.
After adjusting for differences in the age structure between the two populations, the gap in participation rates between Indigenous women and non-Indigenous women aged 40 and over decreased between 2006–2007 and 2019–2020 – from 15.2 percentage points (age-standardised rate of 19.0% for Indigenous women compared with 34.1% for non-Indigenous women) to 7.5 percentage points (23.6% compared with 31.1%). Looking at the decade from 2010–2011 to 2019–20, the gap decreased from 13.4 to 7.5 percentage points.
From 1 July 2013, the target age group for breast screening in Australia changed from 50–69 to 50–74. Time-series data for the 50–69 age group are presented instead of 50–74 to enable comparison over a longer time period. The proportion of Indigenous women aged 50–69 who were screened for breast cancer increased from 29% in 2006–2007 to 38% in 2018–2019. This dropped to 35% in 2019–2020, likely due to the impact of the COVID-19 pandemic from March 2020.
Over the decade from 2010–2011 to 2018–2019, the age-standardised proportion of Indigenous women aged 50–69 who received breast cancer screening increased from 29% to 38%, before declining to 35% in 2019–2020. In contrast, the proportion for non-Indigenous women aged 50–69 remained constant (around 54%) between 2010–2011 and 2018–2019 before declining to 49% in 2019–2020. As a result, there was a 12 percentage point reduction in the gap (from 25 to 14 percentage points) in participation in breast screening between Indigenous and non-Indigenous women from 2010–2011 to 2019–2020 (Table D3.04.12, Figure 3.04.3).
Figure 3.04.3: Age-standardised participation rates and changes in the gap, BreastScreen Australia, women aged 50–69, by Indigenous status, 2006–2007 to 2019–2020
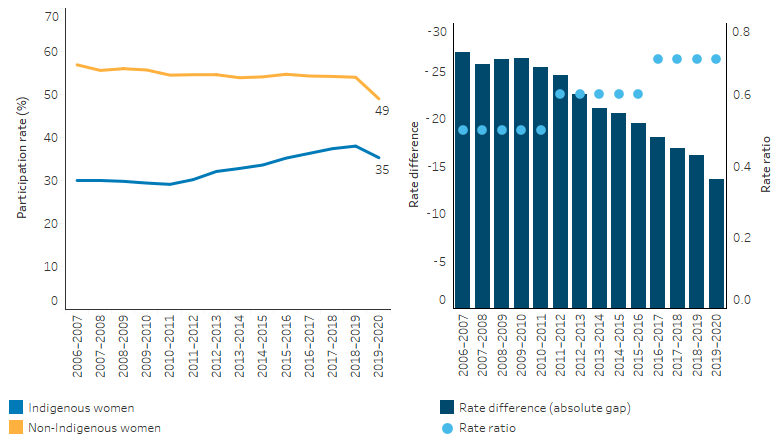
Note: Rate difference is the age-standardised rate (per cent) for Indigenous Australians minus the age-standardised rate (per cent) for non-Indigenous Australians. Rate ratio is the age-standardised rate for Indigenous Australians divided by the age-standardised rate for non-Indigenous Australians.
Source: Table D3.04.12. AIHW analysis of BreastScreen Australia data.
Research and evaluation findings
Participation rates in the NBCSP, BreastScreen Australia and the NCSP appear to be lower for Indigenous Australians than non-Indigenous Australians. Further, the Indigenous death rates among each target age cohort is higher for the cancers these programs are trying to prevent (AIHW 2021b, 2021c)
Several preventable cancers occur more commonly and with lower survival rates for Indigenous than other Australians, indicating that preventive strategies and clinical care are not as effective as they could, and should, be for Indigenous Australians (Clinical Principal Committee Standing Committee on Screening 2018; Condon 2004).
Various studies have investigated the stage of diagnosis and survival rates for cancer for Indigenous Australians. One study in the Northern Territory found that:
- Indigenous Australians were more likely than non-Indigenous Australians to be diagnosed with advanced disease for cancers of the bowel (colorectal), breast, cervix and non-Hodgkin lymphoma. However, for cancer of the lung, Indigenous Australians were more likely to be diagnosed with localised disease (i.e., the cancer had not yet spread). This is possibly because many older Indigenous people have regular chest x-rays for the clinical management of chronic respiratory diseases and as part of contact tracing and long-term follow-up by the tuberculosis control program.
- Indigenous Australians had a lower cancer survival rate than non-Indigenous Australians for all five cancer sites studied. The difference in age-stage-adjusted five-year survival rates was greatest for non-Hodgkin lymphoma (16% for Indigenous Australian compared with non-Indigenous 65%) and least for lung cancer (5% compared with 12%, respectively). With few exceptions, Indigenous Australians had a lower survival rate than non-Indigenous Australians with the same stage at diagnosis for each cancer site.
- Compared with non-Indigenous Australians diagnosed with the same type of cancer, Indigenous Australians are doubly disadvantaged because they are not only diagnosed later, with more advanced disease, but also have a lower survival rate for every stage at diagnosis (Clinical Principal Committee Standing Committee on Screening 2018; Condon et al. 2005).
A study of 815 Indigenous and 810 non-Indigenous patients diagnosed with cancer in Queensland between 1997 and 2002 found that after adjustment for stage at diagnosis, treatment and comorbidities, non-Indigenous patients had a better survival rate than Indigenous patients. The stage at diagnosis was significantly different, with 47% of Indigenous patients diagnosed with localised cancers compared with 53% of non-Indigenous patients. Comorbidities such as diabetes or chronic renal disease were more common in Indigenous patients. Indigenous patients were less likely to have had treatment for cancer (surgery, chemotherapy or radiotherapy) and waited longer for surgery than non-Indigenous patients (Valery et al. 2006).
One study showed that the major limitation in the bowel cancer-screening program is the low participation rate. Therefore, GPs play a crucial role in the success of screening by facilitating participation in the screening program. The study highlighted that the screening of patients with symptoms is inappropriate. Instead, the study recommended that these patients should be referred for investigation of their symptoms (Parkin et al. 2018).
A literature review identified barriers for Indigenous participation in bowel/colorectal cancer-screening programs, some of which appear to be unique to Indigenous people. The review studied the indigenous populations of Canada, New Zealand, Australia and the United States. The review found that indigenous populations have common barriers for screening, such as lack of access to culturally competent health services, discrimination, distrust of Western medicine and distrust of screening tests (D'onise et al. 2020).
Another study examined the delivery of recommended preventive services for Indigenous Australians and investigated the influence of health service and client level factors on adherence to best practice guidelines. The study highlighted that the delivery of recommended preventive care varied widely between different preventive services, with good delivery of most basic measurements but poor follow-up of abnormal findings. The study found that health service characteristics associated with higher quality care were found in the Northern Territory, urban services and centres that serve smaller populations. The study also found that client factors associated with higher quality care included ages between 25 and 34, being female and more regular attendance. The study provided insights for improving the quality of preventive care for Indigenous Australians and highlighted the benefit of Continuous Quality Improvement processes in identifying and addressing areas for improved service delivery (Bailie C et al. 2016).
Indigenous Australian women have a higher incidence of cervical cancer and poorer outcomes for breast and cervical cancer than non-Indigenous women. One small study aimed to implement and evaluate strategies to improve the early detection of breast and cervical cancer by GPs. In three sites a female Indigenous worker and female GP developed and implemented local plans aimed to improve service coordination and access, GP knowledge, recall systems, and health promotion. The study found that important factors in project success included collaboration between service providers, community participation in planning and delivery, having an Indigenous health worker to raise awareness among both the women and GPs and a female GP providing a holistic service (Reath & Carey 2008).
A systematic review of cancer studies explored knowledge, attitudes and behaviours towards cancer screening among indigenous people worldwide. Cancer death among indigenous people is increasing, but these populations commonly under-use cancer-screening services. The review found that knowledge of and participation in screening was greater for breast cancer than for other cancers. It also found that indigenous people tended to have less knowledge, less favourable attitudes, and a higher propensity to refuse screening than non-indigenous populations. The review suggested that greater understanding of knowledge, attitudes and behaviours towards cancer screening in diverse indigenous cultures is needed so that culturally appropriate cancer prevention programs can be provided (Kolahdooz et al. 2014).
A qualitative study of three communities in rural and remote areas of NSW provides insight into both barriers and enablers to healthcare access for Indigenous Australians at all levels of the healthcare system. The study identified six themes which impacts access to health care services: (1) improved coordination of healthcare services; (2) better communication between healthcare services and patients; (3) trust in the service provider and experience of cultural safety; (4) the importance of prioritising health services towards key personal and community issues as defined by Aboriginal people; (5) the importance of reliable, affordable and sustainable healthcare services; (6) distance and transport availability (Nolan-Isles et al. 2021).
Implications
Early detection and early treatment through primary health care has significant benefits for those at risk of disease. Identification of Indigenous patients is the first step in providing access to Indigenous-specific health initiatives, including additional MBS and PBS items, and immunisations. Improving the follow-up of abnormal clinical results and access to referral services is also critical to achieving the benefits of health assessments and screening programs (Bailie C et al. 2016; Bailie J et al. 2014; Spurling et al. 2009; Whop et al. 2016).
Determining the patient’s risk, providing education, encouraging screening and instituting prompt referrals are essential in reducing bowel/colorectal cancer morbidity and mortality (Parkin et al. 2018). Bowel cancer is the fourth most common cancer among Indigenous Australians. Although Indigenous Australians had lower incidence rates of bowel cancer than non-Indigenous Australians, the survival rates were lower and mortality rates were higher (AIHW 2021d). Indigenous Australians are less likely to participate in the bowel cancer-screening program and, of those that are screened, they are more likely to receive a potentially abnormal result and are less likely to have a follow-up colonoscopy. This explains, in part, why Indigenous Australians, when diagnosed, are more likely to have more advanced stages of illness.
More systematic research is required to understand whether the Indigenous participation rates in screening are lower because of less opportunity to screen, less propensity to screen even with the same opportunity or as a consequence of the under-reporting of Indigenous status in screening data. A greater understanding of barriers and enablers affecting participation is needed (D'onise et al. 2020).
Given the lower Indigenous participation rates in breast, bowel and cervical cancer-screening programs, better ways of encouraging regular screening are needed (Christou et al. 2010). In the 2014–15 Budget, the Australian Government committed to accelerating the expansion of the National Bowel Cancer Screening Program with the rollout of a biennial bowel screening interval for all Australians aged 50–74 by 2020.
Indigenous Australian women have a higher incidence of cervical cancer and poorer outcomes for breast and cervical cancer than non-Indigenous women. They also appear to be under-screened. Studies have shown that GPs play a critical role in improving early the detection and management of these conditions among Indigenous Australian women. Interventions such as local partnership approaches that improve service collaboration, GP awareness, recall systems and health promotion could assist in improving participation in screening for breast and cervical cancer. Partnerships involving community members planning and implementing evidence-based strategies may also improve the participation of Indigenous Australian women in breast and cervical cancer screening (Reath & Carey 2008).
Cervical screening will remain vital for many decades because the current HPV vaccines are not effective against all types of the virus that cause cervical cancer. A barrier to reporting on the national cervical screening rate for Indigenous women is that Indigenous status information is not collected on pathology forms in all jurisdictions.
In 2022, the Department of Health and Aged Care (DOHAC) published a series of NCSP information resources (translated into 6 different Indigenous languages) and a video to explain cervical screening to Indigenous Australian women.
The NBCSP also provides information designed for Indigenous Australians, to improve screening participation. In 2018–2019, DOHAC funded the Menzies School of Health Research to develop the National Indigenous Bowel Screening Pilot aimed at encouraging Indigenous Australians to do the bowel screening test, and provided resources for families, communities, and primary health care professionals participating in the pilot program. The pilot tested whether an ‘Alternative Pathway’ using primary health care centres would increase screening participation compared with the usual NBCSP mail-out pathway. The final report of the pilot program found that Indigenous participation through the Alternative Pathway (39.8%) was significantly higher than that of Indigenous Australians in the usual pathway (23.3%), and at a similar rate to that of non-Indigenous Australians (40.6%). Similar screening patterns for the Alternative Pathway were found even in remote areas, where barriers to screening are particularly challenging (Garvey et al. 2020).
Further study is required into factors determining adherence to best practice guidelines and improving the quality of preventive care for Indigenous Australians. Improvement may be achieved by addressing physical, social and cultural barriers to accessing preventive care, and by strengthening systems for the follow-up and completion of preventive health assessments. Possible improvements could also be achieved through health service improvements such as resourcing, team structure and function, and the use of clinical information systems (Bailie C et al. 2016).
Exploring the experience of Indigenous Australians and their outcomes in relation to cancer incidence, stage of disease at presentation, access to treatment and survival can help illustrate aspects of Indigenous Australians’ access to and interaction with the health system. This provides an opportunity to monitor health system performance for Indigenous Australians in relation to both primary care and specialist services, and the interaction between them (Condon 2004).
Implementation of the Health Plan aims to drive structural reform towards models of care that are prevention and early intervention focused, with greater integration of care systems and pathways across primary, secondary and tertiary care. It also emphasises the need for mainstream services to address racism and provide culturally safe and responsive care, and be accountable to Aboriginal and Torres Strait Islander people and communities.
The Health Plan suggests that efforts should be targeted at providing strengths based, culturally safe and holistic, affordable services to ensure early intervention across the life course. Vital to manage the development or progression of health conditions over time, early intervention must focus on the conditions with the potential to become serious, but that are preventable and/or easily treatable. Early intervention priorities may differ between communities depending on their location. Therefore, place-based approaches must be locally determined and embed multidisciplinary care and partnerships. They must include pathways through primary health care (including identification of symptoms, diagnosis, treatment and follow-up care) to allied, specialist and tertiary care.
Objective 5.6 of the Health Plan aims to deliver targeted action to improve cancer screening rates and care pathways for treatment, this includes provision of culturally safe and responsive screening services, improving service accessibility, providing culturally safe information, and implementing community-driven awareness raising activities. The National Aboriginal and Torres Strait Islander Cancer Framework and the Optimal Care Pathway (OCP) for Aboriginal and Torres Strait Islander people with cancer must also continue to be implemented to drive access to culturally safe and responsive cancer treatment and care, including by addressing barriers to identifying, treating and managing cancer.
The policy context is at Policies and strategies.
References
-
AIHW (Australian Institute of Health and Welfare) 2021a. National Cervical Screening Program monitoring report. Vol. CAN 141 (ed., AIHW). Canberra: Australian Government.
-
AIHW 2021b. National Bowel Cancer Screening Program monitoring report 2021. Vol. CAN 139 (ed., AIHW). Canberra: Australian Government.
-
AIHW 2021c. BreastScreen Australia monitoring report 2021. Vol. CAN 140 (ed., AIHW). Canberra: Australian Government.
-
AIHW 2021d. Cancer in Australia 2021. Canberra: AIHW.
-
Bailie C, Matthews V, Bailie J, Burgess P, Copley K, Kennedy C et al. 2016. Determinants and Gaps in Preventive Care Delivery for Indigenous Australians: A Cross-sectional Analysis. Frontiers in public health 4:34.
-
Bailie J, Schierhout G, Kelaher M, Laycock A, Percival N, O’Donoghue L et al. 2014. Follow-up of Indigenous-specific health assessments — a socioecological analysis. The Medical Journal of Australia 200:653-7.
-
Christou A, Katzenellenbogen J & Thompson S 2010. Australia's national bowel cancer screening program: does it work for Indigenous Australians? BMC Public Health 10:21.
-
Clinical Principal Committee Standing Committee on Screening 2018. Population based Screening framework. (ed., Health Do). Canberra: Department of Health.
-
Condon JR 2004. Cancer, health services and Indigenous Australians. Department of Health and Ageing.
-
Condon JR, Armstrong BK, Barnes T & Zhao Y 2005. Cancer incidence and survival for Indigenous Australians in the Northern Territory. Australian and New Zealand journal of public health 29:123-8.
-
D'onise K, Iacobini ET & Canuto KJ 2020. Colorectal cancer screening using faecal occult blood tests for Indigenous adults: A systematic literature review of barriers, enablers and implemented strategies. Preventive Medicine 134:106018.
-
DoH (Australian Government Department of Health) 2020a. National cervical screening program. Viewed 8/7/2020.
-
DoH 2020b. Breastscreen. Department of Health. Viewed 8/7/2020.
-
DoH 2020c. Bowel cancer screening. Viewed 8/7/2020.
-
Garvey G, Brands J, Tighe B, Westby M & Arley B 2020. National Indigenous Bowel Screening Pilot - FINAL REPORT. Department of Health and Aged Care.
-
Jamison DT, Gelband H, Horton S, Jha P, Laxminarayan R, Mock CN et al. 2017. Disease Control Priorities, (Volume 9): Improving Health and Reducing Poverty. The World Bank.
-
Jamison DT, Mosley WH, Measham AR & Bobadilla JL 1993. Disease control priorities in developing countries: a summary. The World Bank.
-
Kolahdooz F, Jang SL, Corriveau A, Gotay C, Johnston N & Sharma S 2014. Knowledge, attitudes, and behaviours towards cancer screening in indigenous populations: a systematic review. The Lancet Oncology 15:e504-e16.
-
Nolan-Isles D, Macniven R, Hunter K, Gwynn J, Lincoln M, Moir R et al. 2021. Enablers and Barriers to Accessing Healthcare Services for Aboriginal People in New South Wales, Australia. Int J Environ Res Public Health 18.
-
Parkin CJ, Bell SW & Mirbagheri N 2018. Colorectal cancer screening in Australia. Australian Journal of General Practice 47:859.
-
Reath J & Carey M 2008. Breast and cervical cancer in Indigenous women: overcoming barriers to early detection. Australian Family Physician 37:178.
-
Spurling G, Hayman NE & Cooney AL 2009. Adult health checks for Indigenous Australians: the first year's experience from the Inala Indigenous Health Service. The Medical Journal of Australia 190:562-4.
-
Valery P, Coory M, Stirling J & Green AC 2006. Cancer diagnosis, treatment, and survival in Indigenous and non-Indigenous Australians: a matched cohort study. The Lancet 367:1842-8.
-
Whop LJ, Baade P, Garvey G, Cunningham J, Brotherton JML, Lokuge K et al. 2016. Cervical Abnormalities Are More Common among Indigenous than Other Australian Women: A Retrospective Record-Linkage Study, 2000–2011. PloS one 11:e0150473.
-
Zwar N & Ackermann E 2016. Guidelines for preventive activities in general practice, 2016, The Royal Australian College of General Practitioners. The Royal Australian College of General Practitioners.

